Ultrasound-guided radiofrequency ablation for the treatment of papillary thyroid carcinoma: a review of the current state and future perspectives
Article information
Abstract
Papillary thyroid carcinoma (PTC) is a highly prevalent cancer that typically exhibits indolent behavior and is associated with a favorable prognosis. The treatment of choice is surgical intervention; however, this approach carries the risk of complications, including scarring and loss of thyroid function. Although active surveillance can mitigate the risk of PTC overtreatment, the possibility of tumor growth and metastasis can elicit anxiety among patients. Ultrasound-guided thermal ablation has emerged as a safe and effective alternative for individuals who are ineligible for or decline surgery. This article provides a review of the clinical research on radiofrequency ablation as a treatment for PTC, offering a thorough examination of its efficacy, safety, and future perspectives.
Introduction
Thyroid cancer is the most common endocrine malignancy [1,2]. Papillary thyroid carcinoma (PTC) represents approximately 80% of all thyroid cancer cases [3] and is typically characterized by its indolent nature and favorable prognosis. Current guidelines [4-7] primarily recommend surgical intervention as the treatment of choice for PTC. However, surgery can lead to complications, such as permanent recurrent laryngeal nerve injury, hypoparathyroidism, scarring, and hypothyroidism necessitating thyroxine replacement therapy. These conditions may persist for a lifetime and can reduce patients’ quality of life [8,9]. To avoid overtreatment of PTC, active surveillance (AS) has been recommended [10]; however, some patients may prefer an alternative. Notably, the choice to perform delayed surgery during AS is often driven by patient anxiety regarding the possibility of tumor growth and metastasis [11-14]. Accordingly, research is exploring less invasive alternatives to surgery beyond AS for the management of PTC.
Increasing attention has been paid to the application of thermal ablation [15] for the treatment of PTC. This minimally invasive approach requires precise placement, which is facilitated by real-time, high-frequency ultrasound (US) guidance [5]. Various percutaneous thermal ablation technologies are commercially available, including radiofrequency ablation (RFA), microwave ablation, laser ablation, and high-intensity focused US [16]. Of these, RFA is a widely adopted method for PTC treatment [17]. Accordingly, the goal of the present article was to review the clinical research pertaining to RFA in the context of PTC and to comprehensively examine its efficacy, safety, and perspectives. This review is intended to serve as a resource to support clinical decision-making regarding PTC treatment.
Evaluation of the Principle, Procedures, and Efficacy of RFA
Principle of RFA
The fundamental mechanism of RFA involves employing a high-frequency alternating current, with wavelengths between 200 and 1,200 kHz, to create an oscillating electric field. As a result, polar macromolecules and charged ions in the tissue adjacent to the electrode needle are driven to vibrate at high speeds, generating frictional heat. Once the temperature reaches 60°C, the affected tissues undergo coagulation necrosis, carbonization, dehydration, and irreversible damage [18]. This process leads to a decrease in tissue volume and ultimately to the absorption of the ablated region [19].
Procedure of RFA
When considering RFA, multidisciplinary consultation should be utilized if available. RFA is recommended for patients who are ineligible for or who decline surgery and AS. Prior to RFA, patients should undergo US examination, computed tomography (CT), US-guided fine-needle aspiration or core needle biopsy, and laboratory examination. Routine US is used to assess the size and location of the tumor, its US characteristics, and its vascularity. CT scans of the neck and chest are conducted to identify any lymph node (LN) involvement or distant metastases. Biopsy samples are analyzed via cytopathological or histopathological evaluation, as well as for the presence of the BRAFV600E mutation. Finally, laboratory tests include assessments of thyroid function and blood coagulation [8].
During RFA, the patient is placed in the supine position with the shoulders properly cushioned and the head tilted back to fully expose the neck. Multi-section US scanning is performed to assess the anatomical relationship between the tumor and the adjacent tissues. Based on this assessment, the RFA protocol is tailored to the tumor’s size and location. Following routine disinfection, 1% lidocaine hydrochloride is applied to the tissue, with US guidance employed to isolate the skin puncture site from the anterior boundary of the thyroid gland. To safeguard critical structures such as the trachea, common carotid artery, and recurrent laryngeal nerve from thermal injury, a protective liquid barrier is created. This is achieved by injecting a suitable volume of liquid—normal saline, 5% glucose, or lidocaine [20]—into the neck’s natural anatomical spaces around the thyroid gland. This injection forms a 5- to 10-mm protective zone that temporarily separates the tumor from these vital structures [21,22]. Next, a safe puncture route is chosen, and an electrode needle is positioned within the tumor under real-time US guidance for the ablation procedure. For larger tumors, the moving-shot technique is employed [23]. This involves segmenting the tumor into multiple small ablation units and then performing edge-overlapping ablation on each unit. In this process, the heat source is moved to avoid thermal damage to nearby tissues and to ensure complete ablation of the tumor. For small tumors, the electrode needle is inserted into the center of the tumor and remains stationary throughout the ablation. During ablation, clinicians should closely monitor vital signs, such as heart rate, blood pressure, and oxygen saturation.
The duration of ablation, as well as the power and energy settings, are determined based on the size and composition of the tumor [24]. For bipolar electrodes, the power is typically set between 3 and 5 W [25,26], whereas other RFA modalities may utilize a higher power, reaching up to 20 W [27]. It is advisable to perform contrast-enhanced US immediately after RFA to assess the ablated area, which generally extends 3-5 mm beyond the tumor edge, to ensure a safe margin and confirm complete ablation [28]. After the procedure, patients are monitored for 1 to 2 hours in the hospital. Any complications that arise during or immediately following ablation are carefully evaluated based on the patient’s clinical signs and symptoms [29].
Several distinctions exist between the RFA procedures for primary PTC and those for recurrence or metastatic LNs. First, the needle insertion pathways differ. For primary PTC, ablations typically employ the trans-isthmic approach, which enables the operator to maintain a stable electrode position, monitor the proximity of the active tip to the recurrent laryngeal nerve, and prevent the leakage of heated ablated material into the perithyroidal area [4]. In contrast, for LNs, the needle insertion path is chosen based on the LN location. Second, differences exist between liquid isolation methods. Ablations for primary PTC involve the creation of a protective barrier between the thyroid tumor and critical structures, whereas for LNs, the barrier is formed around the LN itself. Finally, the ablation techniques themselves vary. For primary PTC, the choice of either the fixed approach or the moving-shot technique is determined based on the tumor size, with the goal of ensuring a safe margin of greater than 3 mm. In contrast, ablations for LNs, which are typically smaller, generally involve a fixed ablation technique to ensure complete eradication.
Assessment of Ablation Efficacy
The effectiveness of RFA is evaluated by examining both primary and secondary endpoints, as well as the technical success of the procedure. The primary endpoint is the disease progression rate (encompassing local recurrence, the development of new tumors, LN metastasis, distant metastasis, or death due to PTC). The secondary endpoints include changes in tumor size and volume, tumor disappearance, technical success, duration of procedure, length of hospital stay, costs associated with hospitalization, and postoperative quality of life. Technical success is defined as the complete absence of enhancement on contrast-enhanced US at the conclusion of the procedure [8].
Complications are documented to assess the safety of RFA. Serious complications include thermal injury to surrounding structures (including the major vessels, esophagus, trachea, brachial plexus, or sympathetic chain), significant hematoma formation, and hemorrhage [30]. The most frequent complications include a sensation of heat during the procedure, as well as pain or discomfort during or after treatment [15]. Vocal changes due to thermal injury to the ipsilateral recurrent laryngeal nerve represent another common and clinically significant complication [31].
RFA for Primary PTC
Single Low-Risk Papillary Thyroid Microcarcinoma
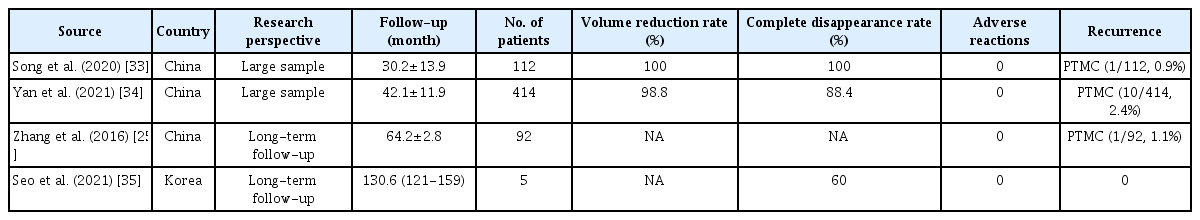
Papillary thyroid microcarcinoma (PTMC) is defined as a PTC with a lesion measuring 10 mm or less in diameter. Dupuy et al. [32] first reported the use of US-guided RFA for thyroid cancer in 2001. Over the course of more than 20 years of ongoing research and advancement, numerous high-quality studies, including investigations with large cohorts and extended follow-up periods (Table 1) [25,33-35], have confirmed the clinical efficacy of RFA for treating single low-risk PTMC. This pertains to cases without clinical evidence of extrathyroidal extension, LN metastasis, or distant metastasis, and without an aggressive histological subtype.
A recent review [27] reported that RFA for low-risk PTMC yields tumor volume reduction rates of 98.5% to 100%, complete disappearance rates ranging from 33.7% to 100%, and tumor progression or recurrence rates between 0% and 4.5%. Two systematic reviews and meta-analyses [15,36], as well as a large-scale matching study [37], revealed no significant differences in postoperative outcomes between RFA and surgery in the treatment of single low-risk PTMC. These outcomes included local tumor progression, LN metastasis, salvage surgery, and recurrence-free survival. However, the rate of complications was significantly higher following surgery than after RFA. Furthermore, RFA has been shown to be significantly superior to surgery in terms of hospitalization costs, length of hospital stay, duration of the procedure, volume of bleeding, and postoperative quality of life [38,39]. It also does not negatively impact subsequent surgical treatments [40]. Collectively, these findings suggest that RFA is a safe and effective treatment for low-risk PTMC and, compared to surgery, may offer a more cost-effective alternative for patients with PTMC who are ineligible for or decline surgery and AS. Nevertheless, it is important to note that most large-scale studies have been conducted in Asia, with relatively few investigations carried out in Western countries.
Multiple Low-Risk PTMCs
According to current guidelines, thermal ablation of thyroid cancer is only indicated for single low-risk PTMC; however, a growing body of research has examined the clinical outcomes of radical RFA for various other PTC types (Table 2) [9,41,42]. These studies, which include cases of bilateral and multiple PTMCs, have yielded encouraging results. Nonetheless, the sample sizes in these investigations were relatively small, and a need exists for large-scale research with long-term follow-up periods to confirm the safety and efficacy of this approach.
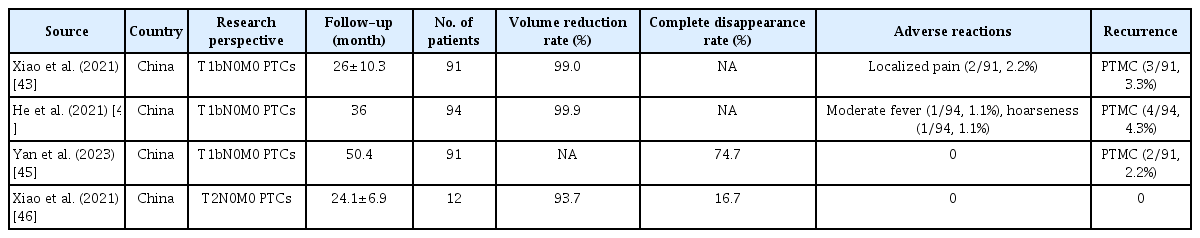
PTCs Exceeding 1 cm
For patients with larger PTCs that do not involve LN metastasis, specifically those classified as T1bN0M0 or T2N0M0, the 2015 American Thyroid Association guidelines [10] recommend lobectomy with isthmic resection rather than total thyroidectomy. Shifts in the guidelines reflect a preference for conservative treatment. Recent research (Table 3) [43-46] indicates that RFA treatment of T1bN0M0 and T2N0M0 PTC may yield outcomes comparable to those for T1aN0M0 PTC. This could be due to the relatively indolent nature of PTC and the similar prognoses for T1a, T1b, and T2 tumors. Therefore, RFA may be a viable alternative treatment option for patients with large PTCs.
RFA for Recurrent and Metastatic PTC
Studies have shown [47-49] that between 10.0% and 30.0% of patients with highly differentiated thyroid cancer experience local recurrence and metastasis following surgical treatment. The anatomical alterations and fibrosis resulting from postoperative scar tissue can impede reoperation and increase the risk of complications. Consequently, current guidelines [4-7] advocate the use of thermal ablation for the radical or palliative treatment of recurrent or metastatic PTC.
Curative Ablation for Locally Recurrent Thyroid Cancer
The European 2021 guidelines [6] for the curative ablation of locally recurrent thyroid cancer indicate that radical ablation is feasible in cases involving three or fewer recurrent PTCs in the neck, each with a diameter of less than 2 cm, and in the absence of distant metastasis. A meta-analysis [50] assessing the efficacy and safety of RFA for locally recurrent and metastatic PTCs reported a tumor volume reduction rate of between 89.5% and 100%, a complete disappearance rate of 68.8%, and an average of only 1.3 ablation sessions required, suggesting the suitability of this approach for patients who are ineligible for or decline surgery. Kim et al. [51] observed no significant differences in 3-year recurrence-free survival rates between RFA and reoperation for locally recurrent PTCs smaller than 2 cm. Furthermore, a recent meta-analysis [52] confirmed that thermal ablation is a safe and effective approach for treating locally recurrent and metastatic PTCs; however, major complications, such as nerve injury, have been reported in up to 12% of cases, particularly when the recurrent foci are in the central neck region. Thus, caution should be exercised before proceeding with ablation of recurrent tumors in the central neck region.
In addition to considering structural changes, it is crucial to evaluate the biochemical response following RFA treatment for recurrent and metastatic PTCs. Serum thyroglobulin (Tg) levels are a sensitive marker for predicting the recurrence and metastasis of thyroid cancer. Moreover, they can serve as an effective indicator of the success of ablation treatment [3,6,53,54]. It is also necessary to account for the influence of anti-Tg antibodies on Tg measurements. Typically, anti-Tg antibody levels transiently rise after surgery as part of an immune response to the procedure, which often results in the underestimation of serum Tg levels in immunometric assays [4].
Palliative Ablation for Recurrent Thyroid Cancer
In cases of recurrent metastatic thyroid cancer that involves invasion of critical structures or presents cosmetic concerns, reducing tumor volume is essential to alleviate symptoms and improve quality of life [55]. To address these conditions, the American Thyroid Association guidelines recommend management strategies that include reoperation, AS, iodine-131 therapy for disease responsive to radioactive iodine, external beam radiation therapy, and various other nonsurgical modalities [56]. Palliative RFA is one example of such a modality. Furthermore, US-guided RFA in conjunction with iodine-125 seed implantation may represent an effective treatment for challenging and severe cases.
Chung et al. [57] reported the efficacy of RFA for the treatment of recurrent thyroid cancer in the central neck area following surgery. They categorized the spatial relationship of all lesions to the trachea, finding that tumors without tracheal invasion had the highest rate of complete disappearance (85.0%). This rate decreased progressively for tumors forming acute, right, and obtuse angles with the trachea, with the lowest rate observed in cases of intraluminal tracheal infiltration. The study reported a relatively high total complication rate of 21.4%, which may be due to the inclusion of tumors close to key cervical structures. Nevertheless, no life-threatening complications or sequelae arose during the follow-up period. Since the therapeutic effectiveness of RFA is inversely related to the extent of tracheal invasion by the tumor, early RFA treatment is advised for recurrent tumors in the central neck region.
US-guided RFA in conjunction with iodine-125 particle implantation frequently improves the local control of metastasis. For challenging and severe cases, including those with lesions protruding from the skin or rupture, this method offers safe and reliable treatment with high clinical utility. Zhai et al. [58] found that US-guided RFA combined with iodine-125 implantation could safely and effectively control local metastatic tumors, while also improving patients’ quality of life. These findings demonstrate the utility of palliative RFA in the management of recurrent and metastatic PTC.
Future Directions
In summary, multiple studies have confirmed the safety and effectiveness of RFA for PTC. Nevertheless, additional research is warranted to improve the detection of occult cervical LN metastases, to more accurately evaluate the aggressiveness of PTC, and to advance ablation technologies.
Diagnosis of Occult Cervical LN Metastasis
Metastasis to cervical LNs is a frequent occurrence in PTC; however, the detection of small metastatic LNs on US presents a diagnostic challenge. Several clinical studies have indicated that contrast-enhanced US may facilitate the early diagnosis of LN metastasis in PTC. Xiao et al. [59] found that the isoenhancement pattern on post-vascular contrast-enhanced US with perfluorobutane was effective in identifying small (short axis diameter, ≤8 mm) cervical lateral LNs with suspected PTC. Zhang et al. [60] reported that contrast-enhanced US lymphography provided a superior diagnostic performance to conventional B-mode US, particularly for LN metastases smaller than 1 cm and for central cervical LN metastases. Accordingly, contrast-enhanced US may represent a new approach for the early detection of LN metastasis in PTC.
Accurate Assessment of the Aggressiveness of PTC
Given the prognostic heterogeneity of PTC, a preoperative determination of its aggressiveness is essential for tailoring treatment to enhance patient prognosis and quality of life. RFA treatment may be suitable for PTCs characterized by low aggressiveness. PTC includes 13 histopathological subtypes; of these, the most aggressive are the tall cell, columnar cell, and hobnail variants, which exhibit unique clinical, pathological, and molecular characteristics [48]. RFA is not recommended for treating these aggressive subtypes. The combined analysis of molecular markers—such as the BRAF, RAS, TERT promoter, RET, and TP53 genes, along with the fusion genes RET/PTC, PAX8/PPARG, and NTRK [61-63]—in conjunction with the application of artificial intelligence [64] may facilitate the accurate evaluation of the aggressiveness, prognostic implications, and recurrence risk of PTC.
New Technologies for Minimally Invasive Therapy
The thyroid gland is surrounded by a complex array of critical structures, including the carotid artery, trachea, esophagus, and nerves. This proximity increases the potential for RFA-induced damage. Consequently, new ablation techniques should be explored and applied. Irreversible electroporation [65] employs high-voltage direct current to generate a strong electric field; this induces the formation of permanent nanoscale fissures in the cell membrane, with subsequent apoptosis and tumor necrosis. This method differs from thermal ablation in that it does not generate heat, thereby preserving tissues that are devoid of cellular components, such as blood vessels and nerves. Clinical studies have confirmed the treatment utility of irreversible electroporation for liver and pancreatic cancers, suggesting that it may represent a viable ablation option, potentially with fewer associated complications than thyroid cancer surgery.
Clear visualization of the target lesion is essential for US-guided RFA. However, US cannot penetrate the bone tissue, compromising the visibility of posterior sternal lesions and key tissue structures. US-CT fusion imaging enables the visualization of lesions that are otherwise obscured by bone tissue. Orlandi et al. [66] first validated the feasibility of RFA in the treatment of large benign thyroid nodules situated behind the sternum, employing US-CT fusion imaging in conjunction with a real-time virtual needle tracking system. This represents a potential alternative approach for the RFA treatment of recurrent and metastatic PTCs located behind the sternum.
High-Level Evidence
Although RFA treatment of PTC has yielded favorable outcomes, most previous studies have been retrospective in nature, with a scarcity of prospective research. Additionally, the literature includes no large-scale multicenter studies with long-term follow-up. With technological advances, such as innovations in cloud computing and big data, it is conceivable that a national or global data management center specifically for thyroid cancer RFA could be developed, along with a long-term follow-up mechanism. Such a center would enable the prediction and monitoring of outcomes following RFA treatment for thyroid cancer and provide robust evidence-based medical insights. This would help ensure the effectiveness of RFA in treating thyroid cancer, supported by standardized indications for its application.
Conclusion
US-guided RFA offers a safe and effective treatment alternative for patients with PTC who are ineligible for or decline surgery. As high-level clinical evidence continues to accumulate and technological advancements are made, the application of RFA in the treatment of PTC is expected to expand.
Notes
Author Contributions
Conceptualization: Zhao GZ, Zhang MB. Data acquisition: Zhao GZ. Data analysis or interpretation: Zhao GZ, Zhang MB. Drafting of the manuscript: Zhao GZ. Critical revision of the manuscript: Zhang MB. Approval of the final version of the manuscript: all authors.
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Key point
Ultrasound-guided thermal ablation represents a safe and effective treatment alternative for patients with papillary thyroid carcinoma who are ineligible for or decline surgery.