AbstractPurposeThe aim of this study was to assess carotid stiffening in a pre-hypertensive (PHT) population using ultrafast pulse wave velocity (ufPWV).
MethodsThis study retrospectively enrolled 626 individuals who underwent clinical interviews, serum tests, and assessments of the systolic blood pressure (SBP), diastolic blood pressure (DBP), carotid intima-media thickness (cIMT), pulse wave velocity-beginning of systole (PWV-BS), and pulse wave velocity-end of systole (PWV-ES) between January 2017 and December 2021. The patients were divided into three groups according to their blood pressure (BP)ŌĆönormal BP (NBP): SBP <130 mmHg and DBP <80 mmHg (n=215); PHT: 130 mmHgŌēżSBP<140 mmHg and/or 80 mmHgŌēżDBP<90 mmHg (n=119); hypertensive (HT): SBP Ōēź140 mmHg and/or DBP Ōēź90 mmHg (n=292). Correlation analyses and comparisons were performed among the groups and in the cIMT subgroups (cIMT Ōēź0.050 cm and <0.050 cm).
ResultscIMT and PWV-ES significantly differed among the BP groups (P<0.05). The BP groups had similar PWV-BS when cIMT <0.050 cm or cIMT Ōēź0.050 cm (all P>0.05). However, the NBP group had a notably lower PWV-ES than the PHT (P<0.001 and P=0.024) and HT (all P<0.001) groups in both cIMT categories, while the PWV-ES in the PHT group were not significantly lower than in the HT group (all P>0.05).
IntroductionHypertension is the most common condition associated with cardiovascular disease (CVD; population attributable fraction of 22.3%) and a known risk factor for mortality [1]. The prevalence of hypertension continues to rise in China, where the number of people with hypertension is expected to reach ~300 million by 2025 [2]. For decades, hypertension was defined as a baseline systolic blood pressure (SBP)/diastolic blood pressure (DBP) of at least 140/90 mmHg [1]. While SBP of 130ŌĆō139 mmHg and DBP of 80ŌĆō89 mmHg were previously defined as "pre-hypertensive," they were redefined as stage I hypertension in the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guidelines [3]. The ACC/AHA guidelines recommend initiating antihypertensive therapy in patients with SBP Ōēź130 or DBP Ōēź80 mmHg to reduce the risk of CVD and cardiovascular events [4]. Indeed, several studies have shown that lowering the SBP to <130 mmHg reduces the risk of fatal outcomes such as myocardial infarction, stroke, and heart failure [5]. However, evidence based on several randomized controlled trials suggested that it was more beneficial to treat patients with office blood pressure (BP) Ōēź140/90 mmHg, leaving the definition of hypertension unchanged (office SBP Ōēź140 mmHg and/or DBP Ōēź90 mmHg) [6]. Moreover, some scholars speculated that the lower BP suggested in the 2017 ACC/AHA guidelines might lead to over-treatment [7]. Whether this "pre-hypertensive" stage differs from the normal and/or hypertensive stage remains unclear, requiring further clarification of the characteristics of individuals with pre-hypertension.
Atherogenesis is a key manifestation of target organ morphological damage, which commonly manifests as coronary heart disease leading to myocardial infarction, cerebrovascular disease leading to stroke and other complications, and biomechanical damage, which manifests as arteriosclerosis. The carotid intima-media thickness (cIMT), measured non-invasively by ultrasonography, is considered a morphological surrogate of early atherosclerosis. Studies have shown that elevated cIMT was associated with obesity, hypertension, and cardiovascular events [8,9]. However, due to the low spatial resolution of current vascular ultrasound probes, cIMT measurements include the intima and media layers together. However, the atherosclerosis process primarily involves the intima layer. Therefore, an increase in cIMT may be primarily due to medial hypertrophy caused by hypertension or aging rather than atherosclerosis-induced intimal hyperplasia [10]. According to current guidelines, risk assessment with cIMT for primary prevention is no longer recommended since research confirmed that the cIMT was inferior to the coronary artery calcification and ankle-brachial index in a medium- to high-risk cohort [11].
Carotid-femoral pulse wave velocity (cfPWV) correlates well with cardiovascular risk factors and mortality and is considered the gold standard for measuring arterial stiffness [12]. The European guidelines include cfPWV in the management of arterial hypertension [13], but its accuracy is limited by the error introduced by the distance and the timing algorithm used. Ultrafast pulse wave velocity (ufPWV) is a novel ultrafast ultrasonographic technique, which directly photographs (>2,000 frames/s) the propagation of the pulse wave to calculate pulse wave velocity in real time [14]. Unaffected by the evaluation error introduced by the distance between measurement points, ufPWV can more accurately characterize the biomechanical properties of the arterial wall and the effect of vascular aging or genetic defects [14]. Moreover, it is an effective and user-friendly alternative for carotid stiffness evaluation in normal individuals and those with relatively early atherosclerosis [15]. Studies have shown that pulse wave velocity-beginning of systole (PWV-BS) and pulse wave velocity-end of systole (PWV-ES) measurements using the ufPWV technique were positively correlated with BP, possibly due to an increase in arterial stiffness linked to hypertension [16]. The authorsŌĆÖ previous studies have shown that ufPWV measurements were an independent predictor of atherosclerosis in patients with hypertension and that PWV-ES could quantitatively evaluate arterial stiffness in healthy individuals, even in those with normal cIMT [17,18]. However, no study has focused on arterial stiffness as quantified with ufPWV in the pre-hypertensive (PHT) population.
Therefore, the aim of this study was to utilize the cIMT and ufPWV to assess the morphological and biomechanical properties of the carotid wall as evaluation of arteriosclerotic characteristics in a PHT population.
Materials and MethodsCompliance with Ethical StandardsThis study was approved by the ethics committee of the Affiliated Hospital of Nanjing University of Chinese Medicine (2017NL-048-02), and the methods were carried out in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients.
Study ParticipantsThis retrospective study included 1,278 consecutive patients who underwent clinical and laboratory examinations and simultaneous BP, cIMT, and ufPWV measurements on the same day between January 2017 and December 2021 at the Jiangsu Provincial Hospital of Chinese Medicine. Data on sex, age, body mass index (BMI), SBP, DBP, total cholesterol (TC), triglyceride (TG), high-density lipoprotein (HDL), low-density lipoprotein (LDL), fasting blood glucose (FBG), hemoglobin (Hb), and creatinine (Cr) were collected. SBP 130ŌĆō139 mmHg and/or DBP 80ŌĆō89 mmHg were defined as pre-hypertension for this study. The exclusion criteria included: (1) incomplete data (n=58); (2) invalid ufPWV measurements (n=31); (3) current smoker (n=224); (4) treatment with any antihypertensive medication within the last 6 months (n=51); (5) cardiovascular events within the last 6 months (n=21); (6) cancer (n=19); (7) FBG Ōēź7.0 mmol/L or diabetes (n=136); (8) renal dysfunction (n=49); and (9) dyslipidemia (n=63). Finally, the included 626 subjects were divided into three BP groupsŌĆöthe normal BP (NBP) group: SBP<130 mmHg and DBP <80 mmHg (n=215); the PHT group: SBP, 130ŌĆō139 mmHg and/or DBP, 80ŌĆō89 mmHg (n=119); and the hypertension (HT) group: SBP Ōēź140 mmHg and/or DBP Ōēź90 mmHg (n=292) (Fig. 1).
BP MeasurementsBP measurements were performed using a regularly-calibrated Omron HEM-7132 electronic sphygmomanometer (Omron, Kyoto, Japan) according to standardized protocols and guidelines for diagnosing hypertension [3,6]. Briefly, patients were asked not to consume caffeine or exercise for 30 minutes and empty their bladder. They were then allowed to relax quietly on a chair for over 5 minutes before the measurements were taken. Clothes that covered the cuffs were removed, the patients placed their arm on the table, and a properly-sized cuff (one that encircled 80% of the arm unless otherwise noted) was placed on the arm at the mid-sternum level, at the level of the heart, with the back and arm supported to avoid muscle contraction and isometric exercise-dependent BP increase. Three BP measurements were recorded 1ŌĆō2 minutes apart, and additional measurements were performed if the first two readings differed by >10 mmHg. The average of the last two BP readings was recorded as the BP.
cIMT and ufPWV MeasurementsUltrasonographic measurements were performed by two physicians with over 15 years of experience to improve the accuracy. Measurements were made with an Aixplorer ultrasound system (SuperSonic Imagine, Aix-en-Provence, France), equipped with an SL10-2 probe (2ŌĆō10 MHz), and operated in the vascular PWV mode. The patients rested supine with their heads tilted slightly backward in an extended position. The patientsŌĆÖ common carotid artery (CCA; including the CCA and the carotid bulb) was scanned along its long axis, visualizing the CCA anterior and posterior walls while avoiding plaque areas and venous structures. A clear and straight section of the posterior carotid artery wall was selected. The width of the sampling frame at the region of interest (ROI) was 1.0 cm. The Aixplorer cIMT automatic measuring system was used to avoid the traditional limitations of cIMT measurement (Fig. 2) [17,18]. The software automatically draws two white dashed lines to track the carotid wall and calculate the average cIMT value for the ROI. A coincidence rate of over 70% was taken as an effective measurement. The measurements were repeated three times to obtain an average cIMT value for each side, and the average of both mean cIMT values was used.
The ufPWV measurements also avoided plaque and venous structures. The subjects held their breath for 5 seconds. A single keystroke was used to automatically obtain a stable image. The yellow ROI box (3.0├Ś3.0 cm) was moved until two red lines automatically tracked the anterior and posterior walls of the CCA [17,18]. The system automatically measured two values at the selected ROI, the PWV-BS and PWV-ES. A variance (╬ö┬▒) of Ōēż2.0 m/s in ufPWV was considered a valid measurement. Three valid ufPWV measurements were averaged, and the mean of the left and right CCA values was used as the final ufPWV. Satisfactory intra-operator reproducibility and inter-operator reproducibility of cIMT and ufPWV measurements were validated in the authorsŌĆÖ previous studies [17,18].
Statistical AnalysisStatistical analysis was performed using IBM SPSS Statistics version 23.0 (IBM Corp., Armonk, NY, USA). Continuous variables are expressed as mean┬▒standard deviation, and categorical variables are presented as numbers (percentages). One-way analysis of variance was used to compare continuous variables among the three groups, and the least significant difference test was used to compare pairs of groups. The chi-square test was used compared categorical variables among the three groups. Pearson correlation coefficients were used to analyze correlations between variables. Scatter plots and regression lines were used for correlation analyses between cIMT, PWV-BS, PWV-ES, and age. Multivariable stepwise linear analysis was performed to assess correlations of clinical characteristics and laboratory findings with PWV-BS and PWV-ES. The candidate variables in the multivariable analysis were age, sex, BMI, SBP, DBP, Hb, FBG, Cr, LDL, HDL, TG, and TC. Bar graphs were used to present the cIMT, PWV-BS, PWV-ES within each group, and a percentage stacked bar graph was used to show the proportion of cIMT among the BP groups. PWV-BS and PWV-ES among the cIMT subgroups and BP groups were compared using clustered bar graphs. To adjust the effect of age on carotid stiffening in the cohort, univariable and multivariable logistic analyses were used to calculate crude (ufPWV only) and adjusted (ufPWV and age) odds ratios with 95% confidence intervals. A P-value of <0.05 was considered statistically significant.
ResultsClinical CharacteristicsThe general characteristics of the NBP, PHT, and HT groups are listed in Table 1. The groups were similar in the sex ratio, LDL, TC, and PWV-BS (P>0.05 for all). Significant differences were noted in age, BMI, SBP, DBP, FBG, Cr, cIMT, and PWV-ES (P<0.001 for all) and HDL (P=0.029), Hb (P=0.039), TG (P=0.005) (Table 1).
Correlations between cIMT, PWV-BS, and PWV-ES and Age
cIMT (r=0.519, P<0.001), PWV-BS (r=0.280, P<0.001), and PWV-ES (r=0.596, P<0.001) were positively correlated with age in all subjects (Fig. 3AŌĆōC). Group analyses showed that of these three variables, PWV-ES had the highest correlation with age in all three BP groups: NBP (r=0.689, P<0.001), PHT (r=0.564, P<0.001), and HT (r=0.445, P<0.001) (Table 2). Multivariable stepwise linear analysis showed that PWV-BS was associated with age (P <0.001, standardized coefficient [STC]=0.282), sex (P=0.030, STC=0.083) and FBG (P=0.035, STC=ŌĆō0.081), while PWV-ES was associated with age (P<0.001, STC=0.568), SBP (P=0.017, STC=0.112), DBP (P=0.043, STC=0.092) and HDL (P=0.020, STC=ŌĆō0.073) (Table 3). These results demonstrated that age was the only and dominant driver of both PWV-BS and PWV-ES in this cohort. Since age was notably distinct among the NBP, PHT and HT populations (Table 1), the following comparisons of carotid stiffening between the groups were thereby adjusted for age.
Comparison of cIMT among the NBP, PHT, and HT Groups
The mean cIMT values in the NBP, PHT, and HT groups were 0.053┬▒0.011 cm, 0.058┬▒0.011 cm, and 0.062┬▒0.011 cm, respectively, with significant differences among them (P<0.001) (Table 1). Inter-group comparisons of cIMT showed significant differences between NBP and PHT (P<0.001), between NBP and HT (P<0.001), and between PHT and HT (P<0.001) (Fig. 4A). The percentage of patients with cIMT Ōēź0.050 cm increased from NBP (26.9%) to PHT (34.1%) to HT (50.0%), with significant differences among the groups (P<0.001) (Fig. 4B).
Comparison of PWV-BS and PWV-ES among the BP Groups
Similar PWV-BS values were found in the NBP, PHT, and HT groups, with cIMT <0.050 cm or Ōēź0.050 cm (Fig. 5A, C). However, PWV-ES in the NBP group differed significantly from the PHT and HT groups (P<0.001 for both; P<0.001 for both adjusted for age), and PHT individuals had a notably lower PWV-ES than HT participants (P=0.002; P=0.017 adjusted for age) (Table 4, Fig. 5B). Furthermore, PWV-ES was significantly lower in the NBP group than in the PHT (P<0.001; P=0.030 adjusted for age) and HT (P<0.001; P<0.001 adjusted for age) groups at cIMT <0.050 cm, and PWV-ES was also lower in the NBP group than in the PHT group (P=0.024; P=0.002 adjusted for age) and HT (P<0.001; P<0.001 adjusted for age) at cIMT Ōēź 0.050 cm, while those in the PHT group were not lower than in the HT group (cIMT <0.050 cm: P=0.134; P=0.063 adjusted for age; cIMT Ōēź0.050 cm: P=0.049; P=0.126 adjusted for age) (Table 4, Fig. 5D).
DiscussionThe results of this study showed that the PHT population was distinctive, with remarkably distinct ufPWV values from healthy individuals and those with hypertension, even when the cIMT was normal and the results were adjusted for age. Furthermore, the present findings indicate that ufPWV could be used for quantitative evaluations of the carotid stiffness in the PHT population, and suggest that biomechanical alterations of atherosclerotic arteries might occur earlier than morphological alterations. The 2017 ACC/AHA guidelines indicated that the prevalence of hypertension had increased observably, and a significant portion of adults taking antihypertensive medicines are recommended for more intensive BP reduction regimens [19]. However, multiple CVD studies have demonstrated that the risk reduction benefit of the target BP stated in the 2017 ACC/AHA guidelines (130/90 mmHg) was lower than the target in the Chinese hypertension guidelines (140/90 mmHg) [20]. Moreover, patients with diabetes or chronic kidney disease and people aged Ōēź60 years might not benefit from lower BP targets and, instead, experience dizziness and cognitive impairment [5,20]. Besides, a recent study in African-Caribbean males aged Ōēź65 years showed that arterial stiffness, quantified by brachial-ankle pulse wave velocity, was markedly higher in PHT individuals than in NBP individuals but indistinguishable from patients with HT [21]. The authorsŌĆÖ previous studies have shown that increases in PWV-ES assessed by ufPWV were consistently synchronized with age, even in a young population of 30ŌĆō39 years old [18]. In summary, a PHT population exists and has different carotid stiffness measured by ufPWV from NBP individuals. The PHT group deserves more attention and specific hypertension management guidelines. Of course, more data and validation of this technique are needed before guidelines can be formulated.
Atherosclerosis is a life-long and multifactorial disease. Besides hypertension, aging is a key risk factor that could drive atherosclerosis development and progression [22,23]. Previous studies have shown that age and high BP were independently associated with the PWV, and measurements of cfPWV showed that age was an important predictor of aortic stiffening [24,25]. ufPWV is an effective, user-friendly alternative for assessing carotid stiffness at a relatively early atherosclerotic stage [15]. Consistent with this stance, the authorsŌĆÖ previous studies have shown that carotid stiffness, measured by ufPWV, was strongly correlated with age and that PWV-ES performed better than PWV-BS at assessing age-related atherosclerosis [18]. These findings are probably due to the following reasons [26,27]: (1) regional PWV-ES can technically be more accurately estimated than PWV-BS; (2) PWV-ES represents the arterial stiffness at the systole phase, which is more effective and sensitive to changes in arterial stiffness due to age and related diseases; and (3) early systolic expansion powered by left ventricular ejection might hinder the detection of minute differences in wall stiffness. This study showed that the standardized coefficients of age in the multivariable linear analyses of PWV-BS and PWV-ES were both notably higher than those of other cardiovascular risk factors, such as sex, SBP and DBP, indicating that aging was a dominant driver of carotid stiffening. Furthermore, PWV-ES in the PHT group was notably higher than in the normal-cIMT NBP group, indicating that ufPWV may be a promising tool for evaluating atherosclerosis progression in a younger population than has been previously done.
Carotid intima thickening is considered an early indicator of atherosclerosis and a target organ for damage caused by hypertension. The cIMT value of patients with hypertension is markedly higher than that in healthy volunteers [28ŌĆō30]. Studies have shown that the carotid stiffness, measured by ufPWV, was positively correlated with cIMT [15,31]. The authorsŌĆÖ previous results demonstrated that cIMT and PWV-ES were higher in patients with hypertension than in healthy people, and changes in cIMT appeared to lag behind PWV-ES when measurements were made with ufPWV [18,32]. These previous findings also demonstrated that arterial stiffening was highly accelerated in the early stages and slowed down thereafter, seemingly reaching an upper limit [18]. This finding could explain the more apparent arterial stiffness differences in participants with normal cIMT (<0.050 cm) in this study, showing a unique ufPWV value when assessing early arteriosclerosis linked to pre-hypertension. This study showed that with an increase in BP, a larger proportion of the population had increased cIMT. The proportion of patients with increased cIMT when using ufPWV in the PHT group was prominently higher than in the NBP and HT groups, confirming that the arterial morphology and stiffness in the PHT population were distinctive. This finding agrees with the aim of the ACC/AHA guideline to merge prevention and treatment, proposing a goal for the category formerly accepted as pre-hypertension [3,7]. However, the question of whether intensive therapy is appropriate for the PHT population remains controversial, requiring further verification and validation in future studies.
There were some limitations to this study. First, there were considerably fewer patients in the PHT group than in the other two groups due to its smaller range of BP. Second, patients with atherosclerosis often have multiple coexisting risk factors that simultaneously affect their disease progression. Therefore, it is usually difficult to control for all the confounding factors. Third, this was a retrospective study that did not screen patients through an age-matching process. Furthermore, atherosclerosis is a life-long disease in which numerous factors play various roles. Some factors that might affect the cIMT and carotid stiffening were not considered in this retrospective study (e.g., perimenopause, family history, lifestyle, and work style). Fourth, the PWV-BS and PWV-ES were measurements representing the arterial stiffness, performed at two time points in the cardiac cycle rather than average values of the arteries of interest, so they may be lower than the values measured when using the cfPWV technology. Therefore, a larger sample in a multi-center prospective cohort study could further explore this approach in the future.
In conclusion, the cIMT (representing morphological) and carotid stiffness (representing biomechanical properties) of patients with PHT were distinctive from those in the NBP and HT groups. ufPWV may be used for the early evaluation of arteriosclerosis, which mainly occurs in the subendothelial space of medium-sized to large arteries at regions of disturbed blood flow or bifurcations and is linked to pre-hypertension.
NotesAuthor Contributions Conceptualization: Ma X, Zhu Z. Data acquisition: Ma X, Wang Y, Shen B, Luan Y, Gao H. Data analysis or interpretation: Ma X, Liu W. Drafting of the manuscript: Ma X, Zhu Z, Huang H. Critical revision of the manuscript: Jiang X, Wu Y, Zou C, Huang H. Approval of the final version of the manuscript: all authors. AcknowledgementsThis work was supported by the National Natural Science Foundation of China (grant number: 81901756), the Key Research and Development Program of Jiangsu Province (grant number: BE2019725), the Research Project of Geriatric Health of Jiangsu Province (grant number: LK2021005), and the Research Project of National Administration of Chinese Medicine (grant number: YB2015020).
References1. Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 2020;395:795ŌĆō808.
2. Huang K, Yang X, Liang F, Liu F, Li J, Xiao Q, et al. Long-term exposure to fine particulate matter and hypertension incidence in China. Hypertension 2019;73:1195ŌĆō1201.
3. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018;138:e426ŌĆōe483.
4. Jaeger BC, Anstey DE, Bress AP, Booth JN 3rd, Butler M, Clark D 3rd, et al. Cardiovascular disease and mortality in adults aged Ōēź60 years according to recommendations by the American College of Cardiology/American Heart Association and American College of Physicians/American Academy of Family Physicians. Hypertension 2019;73:327ŌĆō334.
5. Reboussin DM, Allen NB, Griswold ME, Guallar E, Hong Y, Lackland DT, et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018;138:e595ŌĆōe616.
6. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021ŌĆō3104.
7. Bakris G, Ali W, Parati G. ACC/AHA versus ESC/ESH on hypertension guidelines: JACC Guideline Comparison. J Am Coll Cardiol 2019;73:3018ŌĆō3026.
8. Willeit P, Tschiderer L, Allara E, Reuber K, Seekircher L, Gao L, et al. Carotid intima-media thickness progression as surrogate marker for cardiovascular risk: meta-analysis of 119 clinical trials involving 100 667 patients. Circulation 2020;142:621ŌĆō642.
9. Sun P, Liu L, Liu C, Zhang Y, Yang Y, Qin X, et al. Carotid intimamedia thickness and the risk of first stroke in patients with hypertension. Stroke 2020;51:379ŌĆō386.
10. Xu M, Zhang M, Xu J, Zhu M, Zhang C, Zhang P, et al. The independent and add-on values of radial intima thickness measured by ultrasound biomicroscopy for diagnosis of coronary artery disease. Eur Heart J Cardiovasc Imaging 2019;20:889ŌĆō896.
11. Geisel MH, Bauer M, Hennig F, Hoffmann B, Lehmann N, Mohlenkamp S, et al. Comparison of coronary artery calcification, carotid intima-media thickness and ankle-brachial index for predicting 10-year incident cardiovascular events in the general population. Eur Heart J 2017;38:1815ŌĆō1822.
12. Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant metaanalysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol 2014;63:636ŌĆō646.
13. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013;34:2159ŌĆō2219.
14. Marais L, Pernot M, Khettab H, Tanter M, Messas E, Zidi M, et al. Arterial stiffness assessment by shear wave elastography and Ultrafast pulse wave imaging: comparison with reference techniques in normotensives and hypertensives. Ultrasound Med Biol 2019;45:758ŌĆō772.
15. Pan FS, Yu L, Luo J, Wu RD, Xu M, Liang JY, et al. Carotid artery stiffness assessment by Ultrafast ultrasound imaging: feasibility and potential influencing factors. J Ultrasound Med 2018;37:2759ŌĆō2767.
16. Yang W, Wang Y, Yu Y, Mu L, Kong F, Yang J, et al. Establishing normal reference value of carotid ultrafast pulse wave velocity and evaluating changes on coronary slow flow. Int J Cardiovasc Imaging 2020;36:1931ŌĆō1939.
17. Zhu ZQ, Chen LS, Jiang XZ, Wu YY, Zou C, Luan Y, et al. Absent atherosclerotic risk factors are associated with carotid stiffening quantified with ultrafast ultrasound imaging. Eur Radiol 2021;31:3195ŌĆō3206.
18. Zhu ZQ, Chen LS, Wang H, Liu FM, Luan Y, Wu LL, et al. Carotid stiffness and atherosclerotic risk: non-invasive quantification with ultrafast ultrasound pulse wave velocity. Eur Radiol 2019;29:1507ŌĆō1517.
19. Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT Jr, et al. Potential U. S S;S:SŌĆōS.
20. Li D, Zeng X, Huang Y, Lei H, Li G, Zhang N, et al. Increased risk of hypertension in young adults in southwest China: impact of the 2017 ACC/AHA high blood pressure guideline. Curr Hypertens Rep 2019;21:21.
21. Kuipers AL, Miljkovic I, Barinas-Mitchell E, Cvejkus R, Bunker CH, Wheeler VW, et al. Arterial stiffness and hypertension status in Afro-Caribbean men. J Hypertens 2019;37:546ŌĆō554.
22. Tyrrell DJ, Goldstein DR. Ageing and atherosclerosis: vascular intrinsic and extrinsic factors and potential role of IL-6. Nat Rev Cardiol 2021;18:58ŌĆō68.
23. Hurtubise J, McLellan K, Durr K, Onasanya O, Nwabuko D, Ndisang JF. The different facets of dyslipidemia and hypertension in atherosclerosis. Curr Atheroscler Rep 2016;18:82.
24. Diaz A, Tringler M, Wray S, Ramirez AJ, Cabrera Fischer EI. The effects of age on pulse wave velocity in untreated hypertension. J Clin Hypertens (Greenwich) 2018;20:258ŌĆō265.
25. Logan JG, Barksdale DJ. Pulse wave velocity in Korean American men and women. J Cardiovasc Nurs 2013;28:90ŌĆō96.
26. Hermeling E, Reesink KD, Kornmann LM, Reneman RS, Hoeks AP. The dicrotic notch as alternative time-reference point to measure local pulse wave velocity in the carotid artery by means of ultrasonography. J Hypertens 2009;27:2028ŌĆō2035.
27. Huang C, Su Y, Zhang H, Qian LX, Luo J. Comparison of different pulse waveforms for local pulse wave velocity measurement in healthy and hypertensive common carotid arteries in vivo. Ultrasound Med Biol 2016;42:1111ŌĆō1123.
28. Li X, Jiang J, Zhang H, Wang H, Han D, Zhou Q, et al. Measurement of carotid pulse wave velocity using ultrafast ultrasound imaging in hypertensive patients. J Med Ultrason (2001) 2017;44:183ŌĆō190.
29. Wu Y, Liu F, Adi D, Yang YN, Xie X, Li XM, et al. Association between carotid atherosclerosis and different subtypes of hypertension in adult populations: a multiethnic study in Xinjiang, China. PLoS One 2017;12:e0171791.
30. Zhang L, Fan F, Qi L, Jia J, Yang Y, Li J, et al. The association between carotid intima-media thickness and new-onset hypertension in a Chinese community-based population. BMC Cardiovasc Disord 2019;19:269.
Flow diagram of the study cohort selection.This study enrolled 1,278 consecutive patients who underwent clinical and laboratory examinations and simultaneous BP, cIMT, and ufPWV measurements. After selecting based on the inclusion and exclusion criteria, the 626 included subjects were divided into three BP groups: normal BP (NBP, n=215), pre-hypertensive (PHT, n=119), and hypertensive (HT, n=292). BP, blood pressure; cIMT, carotid intima-media thickness; ufPWV, ultrafast pulse wave velocity; FBG, fasting blood glucose; SBP, systolic blood pressure; DBP, diastolic blood pressure.
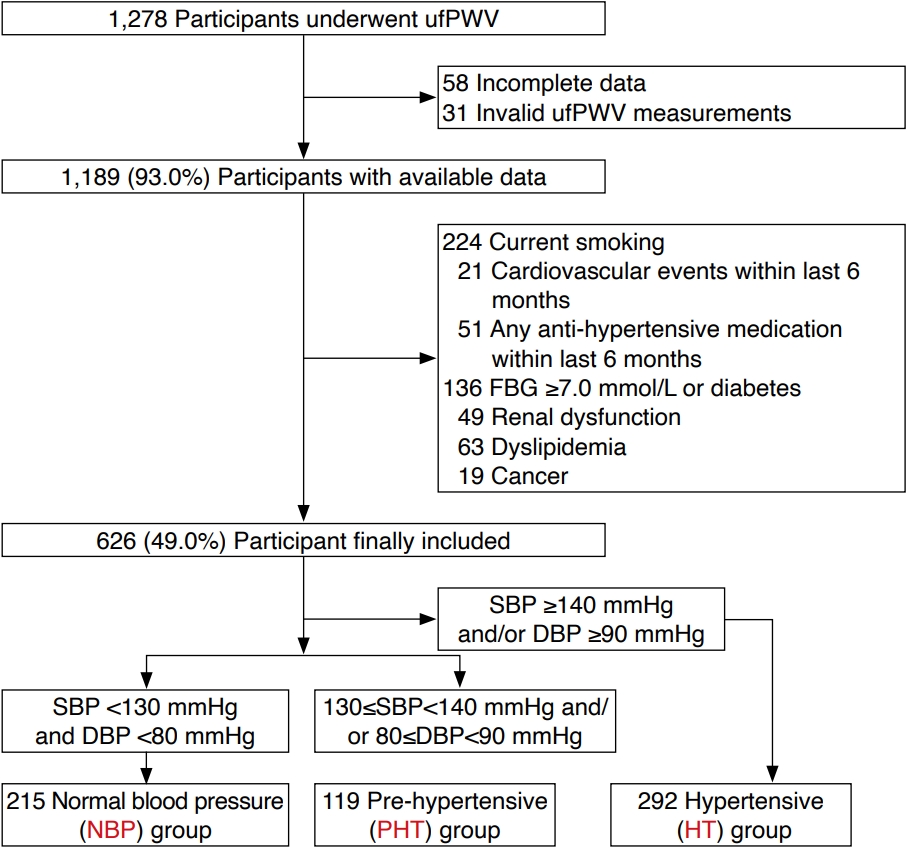 Fig.┬Ā1.Protocols for the assessment of cIMT using ACAMS and carotid stiffness using ufPWVA. Measurement of cIMT was performed by using ACAMS. Utilizing ACAMS, a white ROI box was drawn at the posterior wall of the CCA; the intimal and medial lines of the CCA were automatically recorded with two dotted lines, and the mean cIMT of the ROI was obtained with a fit of 98%. B. PWV-BS and PWV-ES were measured by using ufPWV. Using ufPWV imaging, a yellow ROI box covered and a red line automatically tracked the anterior and posterior walls of the CCA. The PWV-BS and PWV-ES values were calculated in the ROI with ╬ö┬▒ Ōēż2.0 m/s, respectively. cIMT, carotid intima-media thickness; ACAMS, Aixplorer cIMT automatic measuring system; ROI, region of interest; ufPWV, ultrafast pulse wave velocity; CCA, common carotid artery; PWV-BS, pulse wave velocity-beginning of systole; PWV-ES, pulse wave velocityend of systole.
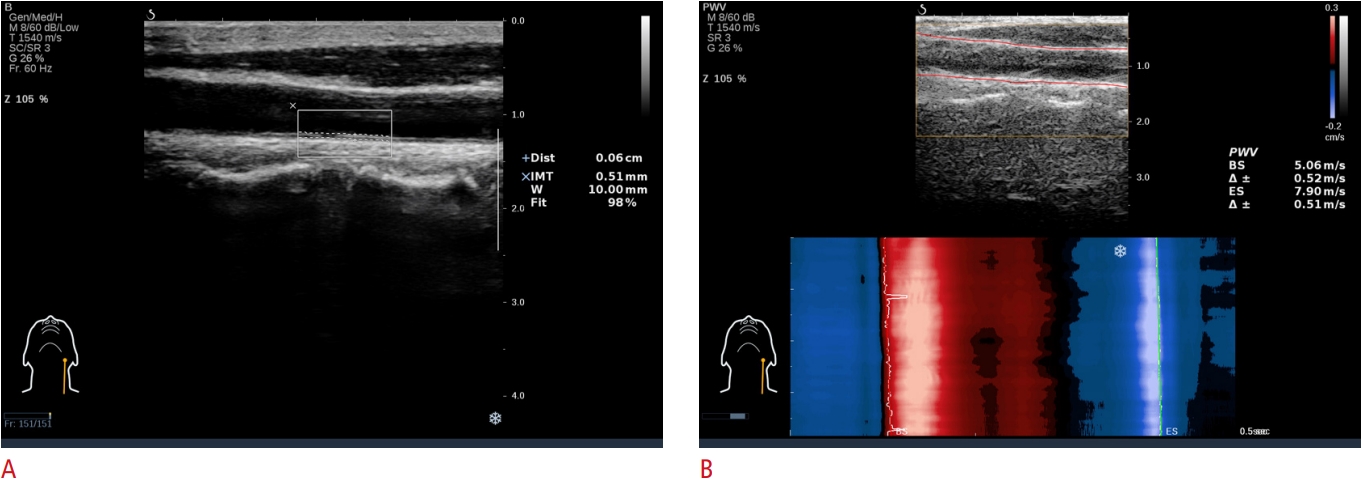 Fig.┬Ā2.Correlations between cIMT, PWV-BS, and PWV-ES and age.PearsonŌĆÖs correlation analysis (n=626) is shown between age and cIMT (r=0.519, P<0.001) (A), PWV-BS (r=0.280, P<0.001) (B), and PWV-ES (r=0.596, P<0.001) (C). cIMT, carotid intima-media thickness; PWV-BS, pulse wave velocity-beginning of systole; PWVES, pulse wave velocity-end of systole.
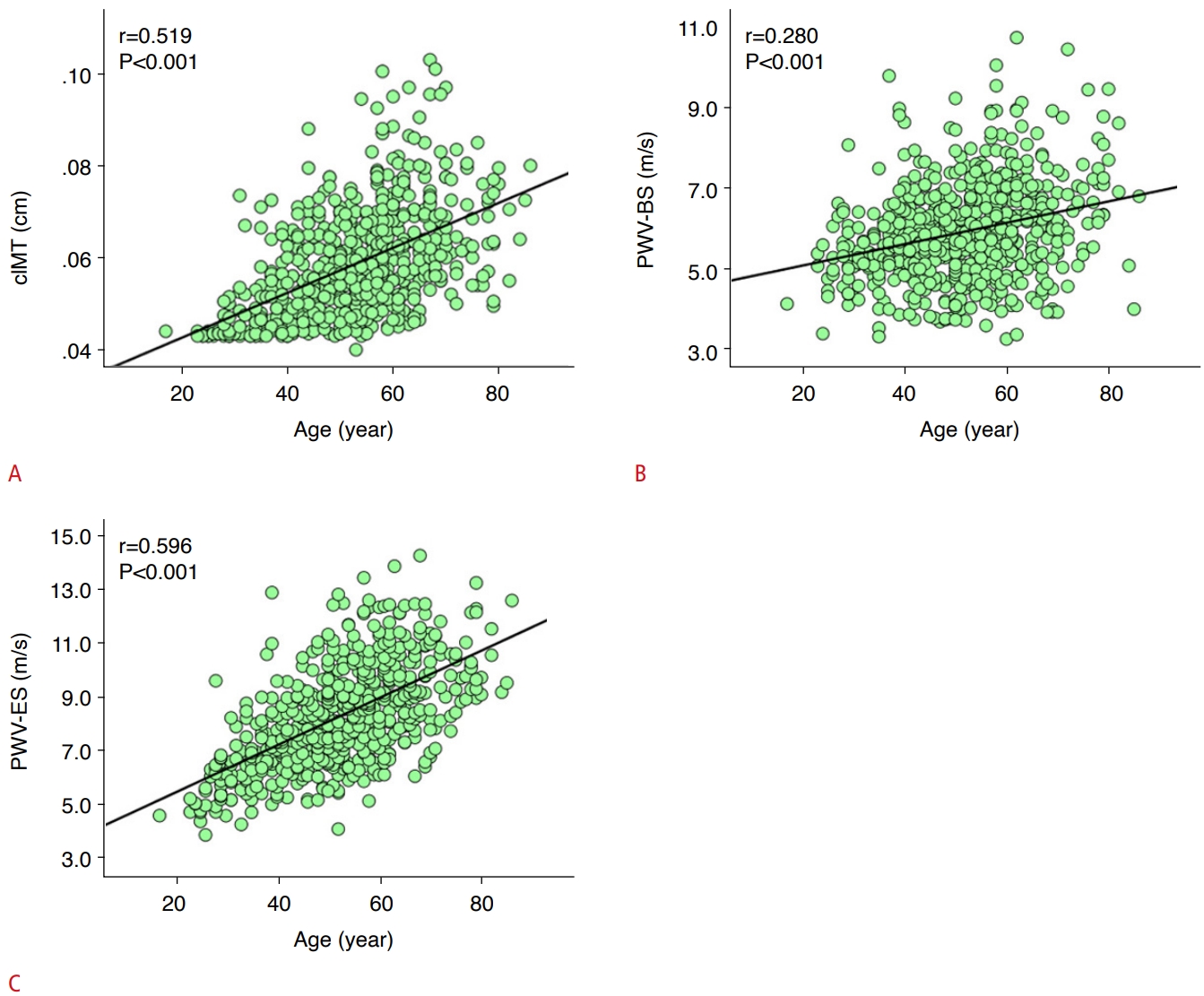 Fig.┬Ā3.Comparison of cIMT among the BP groups.A. Comparisons were made with cIMT among the NBP (n=215), PHT (n=119), and HT (n=292) groups. B. With the cutoff of 0.050 cm by using ACAMS, a comparison of the proportion of thickened cIMT was made among the NBP (n=215), PHT (n=119), and HT (n=292) groups. **P<0.01, ***P<0.001. cIMT, carotid intima-media thickness; BP, blood pressure; NBP, normal blood pressure; PHT, pre-hypertensive; HT, hypertensive; ACAMS, Aixplorer cIMT automatic measuring system.
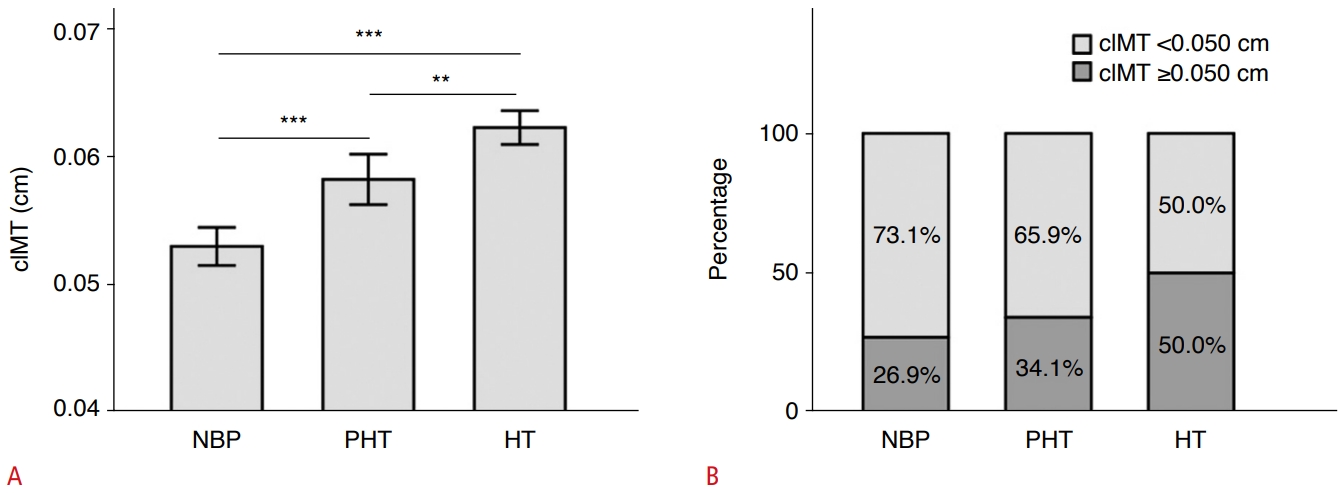 Fig.┬Ā4.Comparison of PWV-BS and PWV-ES among the BP groups and the cIMT subgroups.Comparisons were made with PWV-BS (A) and PWV-ES (B) among the NBP (n=215), PHT (n=119), and HT (n=292) groups in the total population, respectively. Comparisons were made with PWV-BS (C) and PWV-ES (D) among the NBP, PHT, and HT groups in the subpopulations with cIMT <0.050 cm and Ōēź0.050 cm, respectively. Comparison were made among three BP groups according to cIMT subgroups: ***P<0.001; Comparison between two BP groups with age-adjusted P-values: vs. NBP group with #P<0.05, ##P<0.01, ###P<0.001; vs. PHT group with &P<0.05. PWV-BS, pulse wave velocity-beginning of systole; PWV-ES, pulse wave velocity-end of systole; BP, blood pressure; cIMT, carotid intima-media thickness; NBP, normal blood pressure; PHT, pre-hypertensive; HT, hypertensive.
 Fig.┬Ā5.Table┬Ā1.General characteristics of the study population Values are presented as mean┬▒standard deviation or number (%). NBP, normal blood pressure; PHT, pre-hypertensive; HT, hypertensive; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; Hb, hemoglobin; FBG, fasting blood glucose; Cr, creatinine; LDL, low-density lipoprotein; HDL, high-density lipoprotein; TG, triglyceride; TC, total cholesterol; cIMT, carotid intima-media thickness; PWV-BS, pulse wave velocity-beginning of systole; PWV-ES, end-systole pulse wave velocity. Table┬Ā2.Analysis of the correlations between age and cIMT, PWV-BS, and PWV-ES in the NBP, PHT, and HT groups Table┬Ā3.Multivariable stepwise linear regression analysis for PWV-BS and PWV-ES in the total population Significant at P<0.05. PWV-BS, pulse wave velocity-beginning of systole; PWV-ES, end-systole pulse wave velocity; CI, confidence interval; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; Hb, hemoglobin; FBG, fasting blood glucose; Cr, creatinine; LDL, low-density lipoprotein; HDL, high-density lipoprotein; TC, total cholesterol; TG, triglyceride. Table┬Ā4.Univariate and multivariable logistic regression analysis for PWV-BS and PWV-ES among the NBP, PHT, and HT groups in the total population and the cIMT subpopulations All ORs were calculated with the NBP or PHT group as the reference (NBP vs. PHT was calculated with the NBP group as the reference). Crude: PWV-BS or PWV-ES only. Adjusted by age: PWV-BS+age or PWV-ES+age. Significant ORs at P<0.05. PWV-BS, pulse wave velocity-beginning of systole; PWV-ES, end-systole pulse wave velocity; NBP, normal blood pressure; PHT, pre-hypertensive; HT, hypertensive; cIMT, carotid intima-media thickness; OR, odds ratio; CI, confidence interval. |