AbstractPurposeThe goal of this study was to follow benign thyroid nodules confirmed by ultrasound (US)-guided core needle biopsy (CNB) after inconclusive cytology on fine-needle aspiration (FNA) biopsy.
MethodsSixty-two thyroid nodules from 62 patients with CNB-confirmed benign histology that initially had inconclusive cytology on FNA were retrospectively included. The thyroid nodules were followed for 38.7 months (median, 27.5 months; range, 6 to 101 months), and the US findings of biopsied nodules, such as the interval change in size, US characteristics, and imaging category based on the Korean Thyroid Imaging Reporting and Data System (K-TIRADS), were evaluated. In addition, patients’ clinical records were reviewed for any further management or newly diagnosed thyroid malignancy.
Ultrasound (US)-guided fine-needle aspiration (FNA) has been established as the standard biopsy method to diagnose malignancy in thyroid nodules. However, the limitations of FNA are also known, including a considerable rate of inconclusive results, such as non-diagnostic results and atypia of undetermined significance or follicular lesions of undetermined significance (AUS/FLUS) [1]. In addition, the non-diagnostic rate was higher (up to 50%) in cases of repeated FNA and AUS/FLUS cytology, which accounted for 19%-31% of nodules with previous AUS/FLUS FNA readings [2-6]. In prior studies comparing repeated FNA and core needle biopsy (CNB) for nodules initially diagnosed as AUS/FLUS, CNB showed a lower rate of inconclusive results and better diagnostic performance [7]. Therefore, US-guided CNB is widely accepted as an alternative to FNA for indeterminate thyroid nodules [8]. With the revision of the Korean Thyroid Imaging Reporting and Data System (K-TIRADS) in 2021, CNB was added to the management of thyroid nodules with AUS/FLUS cytology. Specifically, the management changed from repeated FNA to repeated FNA "or CNB" within 3-6 or 6-12 months for nodules with high- or intermediate-/low-suspicion K-TIRADS US patterns, respectively [9,10]. However, the natural course of CNB-confirmed benign thyroid nodules remains unclear, and there is not yet a consensus regarding the follow-up management for benign histology after thyroid CNB as an alternative diagnostic tool. The purpose of this study was to investigate the follow-up of benign thyroid nodules, confirmed by US-guided CNB, as an alternative to repeated FNA for inconclusive cytological results on previous FNA.
This study was approved by an institutional review board of our institution (Hanyang University Hospital 2020-05-022-001). The need for informed consent for the CNB procedure was waived due to the retrospective nature of this study.
From June 2010 to November 2020, US-guided CNB was performed for 337 thyroid nodules in 335 consecutive patients. Among them, 183 thyroid nodules (54.3%) had benign histology confirmed by CNB. The exclusion criteria were as follows: (1) thyroid nodules with initial conclusive FNA cytology results (n=45), (2) first-line CNB (n=32), (3) nodules lost to follow-up (n=43), and (4) nodules that went on to receive surgery immediately after the CNB procedure (n=1). Finally, 62 thyroid nodules with initial inconclusive FNA cytology (Bethesda category I or III) from 62 patients (45 women and 17 men) were included in this study. The mean age of the patients was 53 years (range, 25 to 80 years). The demographics of the study population are shown in Table 1.
US images were obtained using 12- or 15-MHz linear-array transducers from three vendors (Philips, Bothell, WA, USA; Supersonic Imagine, Aix-en-Provence, France; and Samsung Medison Co., Seoul, Korea). The scanning protocol included ≥2 orthogonal images, such as transverse and longitudinal images, from each thyroid nodule. US imaging was performed by one of four radiologists with 5 to 20 years of experience.
US-guided FNA was performed by the same radiologist who evaluated the thyroid gland. Using a 21- to 25-gauge needle, once or twice, they obtained the specimen by a perpendicular or parallel approach with a combination of the aspiration technique and capillary technique depending on the characteristics of the thyroid nodule. The aspiration technique refers to the "to-and-fro" needle movement with 2–3 mL of suction applied. The FNA results were interpreted by three pathologists according to the Bethesda categories for reporting thyroid cytopathology.
US-guided CNB was also performed by the same radiologists who evaluated the thyroid gland. The CNB procedures were performed by one of two radiologists with >5 years of CNB experience using a disposable 18-gauge, single-action spring-activated needle and a guiding needle. They obtained two samples from each lesion. After the biopsy, each patient manually self-compressed the biopsy site for 10–20 minutes. From 2010 to 2015, the CNB results were interpreted by institutional consensus among three pathologists, and "pathological benign nodules" were defined as thyroiditis, adenomatous hyperplasia, or benign adenomatoid nodule. Since 2015, a six-tier pathology reporting system has been used according to guidelines published by the Korean Endocrine Pathology Thyroid CNB Study Group. The six categories are non-diagnostic, benign, indeterminate, follicular neoplasm/suspicious for a follicular neoplasm, suspicious for malignancy, and malignant [11].
Two experienced radiologists with 10-20 and 5-15 years of experience in thyroid US and interventional procedures, respectively, reviewed the US findings of the initial and follow-up examinations in consensus. The interval change in the size was verified in three dimensions. A significant interval growth was defined as a 20% increase in two or more dimensions and a minimal increase of 2 mm related to the length measured when CNB was performed. The occurrence of any interval change in the US characteristics and the K-TIRADS categories of the thyroid nodules was evaluated. The US characteristics were assessed based on the K-TIRADS, including the internal components, echogenicity, size, margin, shape, orientation, and calcification of the nodules. The internal components were classified based on the proportion of cystic tissue; then, the nodules were separated into three categories based on whether they were predominantly cystic, predominantly solid, or solid. The echogenicity findings were compared to the thyroid parenchyma and classified as hypoechoic, isoechoic, or hyperechoic. Isolated calcifications were separately described. The margin was categorized as smooth, spiculated/microlobulated, or ill-defined. The shape of the nodule was classified as round to oval or irregular (neither round nor oval). The orientation was categorized as parallel (when the anteroposterior diameter was shorter than or equal to the transverse or longitudinal diameter) or non-parallel (when the anteroposterior diameter was longer than the transverse or longitudinal diameter on transverse or longitudinal images). The presence of calcifications was evaluated; when present, the category was divided into microcalcifications (echogenic foci ≤1 mm) and macrocalcifications (echogenic foci >1 mm in size). Suspicious US features for malignancy were defined as spiculated/microlobulated margins, microcalcifications, and a non-parallel orientation [10]. The clinical records of these patients and their surgical histology during follow-up were also reviewed.
The mean size of the thyroid nodules was 16.8±11.0 mm (range, 4 to 53 mm). Of the 62 thyroid nodules, 20 nodules (32.5%) were <10 mm. The K-TIRADS category was 3 (low suspicion) in 32 (51.6%) nodules, 4 (intermediate suspicion) in 22 (35.5%) nodules, and five (high suspicion) in eight (12.9%) nodules. The US findings of the thyroid nodules are listed in Table 2.
After biopsy, the US exams followed at an interval of 6-12 months. The mean follow-up duration was 38.7±27.5 months, ranging from 6 to 101 months.
The follow-up results of the nodules according to initial cytological reports are arranged in Fig. 1. Among these patients, three (4.8%) showed interval growth; the mean interval growth was 52.3% (range, 45.5% to 61.5%) in each nodule dimension (Fig. 2). All garnered low suspicion (K-TIRADS 3) on the initial US examination, and this did not change according to any characteristics of the nodule throughout the follow-up period. There was no upgrade of the K-TIRADS category during the follow-up US studies, and five cases were downgraded to a lower K-TIRADS category during the US follow-up period. All five of these cases were histologically proven thyroiditis that improved over time (Fig. 3).
The characteristics of eight cases with high suspicion (K-TIRADS 5) upon initial US are listed in Table 3. Four cases were histologically proven thyroiditis, and three lesions disappeared during follow-up. The others were stable without any changes in the US characteristics or interval growth.
In this study, three of 62 thyroid nodules (4.8%) showed interval growth, and the characteristics of those cases are listed in Table 4. One case underwent repeated CNB and exhibited benign histology.
During the follow-up period, there were no cases of newly diagnosed malignancy.
This study followed benign thyroid nodules confirmed by US-guided CNB as an alternative to repeated FNA for inconclusive thyroid nodules on previous FNA.
To the best of the authors’ knowledge, no existing research on the natural course of CNB-confirmed benign thyroid nodules with inconclusive cytology has been published. The interval growth of cytologically benign thyroid nodules has been evaluated by only a few studies that have shown a poor correlation between nodule growth and malignancy [12-14]. Most of the benign thyroid nodules increased in size without evidence of malignant transformation. In one study by Lee et al. [15], the malignancy rate of minimally cystic thyroid nodules was significantly lower than that of pure solid nodules and slightly higher than that of partially cystic nodules, meaning that the presence of more cystic components can be considered a benign characteristic. In previous reports, the most commonly reported US changes were cystic changes, margin changes, and calcification pattern changes, in descending order of frequency [14]. The present study revealed a rate of 7.7% (5/65) for cystic change, and there was no definite change in the margins or calcification patterns during the follow-up period. Among 62 cases, three cases (4.8%) showed interval size growth, while 59 (95.2%) demonstrated no interval change or decrease in size. There was no upgrade of the K-TIRADS category or newly diagnosed malignancy during the follow-up period. As the patients included in this study underwent CNB after initial FNA, the cystic contents had been aspirated before. Therefore, changes in internal content were less common during follow-up than reported in previous studies regarding follow-up of benign thyroid FNA. Furthermore, long-term follow-up of a large series would be necessary to validate the malignancy rate of CNB-confirmed benign thyroid nodules.
This study used the definition of inconclusive results as a combination of Bethesda categories I and III. According to the study by Ha et al. [1], a higher conclusive diagnosis rate was obtained when Bethesda categories I and III rather than Bethesda categories I, III, and IV were considered as inconclusive. Therefore, the diagnostic performance of this study is quite reliable.
The benign category (category II) of CNB histology contains benign follicular nodules, (including nodular hyperplasia, follicular adenoma, colloid nodules, and nodules in Graves disease), Hashimoto’s thyroiditis, and subacute granulomatous thyroiditis. Among these, thyroiditis has suspicious US findings and can be categorized as K-TIRADS 4 or 5. Typical findings of ill-defined, irregular, geographical hypoechogenicity could be helpful in the differential diagnosis of malignancy; however, biopsy and further follow-up are still recommended [11]. The CNB results in this study revealed 13 cases of thyroiditis. These lesions disappeared or markedly decreased in size on follow-up US within 6-12 months.
FNA-proven benign thyroid nodules with suspicious US features had a somewhat high false-negative rate, ranging from 13.6% to 56.6% [10,16-21]. According to previous reports, the malignancy rate in cases with benign histology on thyroid CNB has been reported to range from 0.0% to 7.7% (Table 5). The false-negative rate of thyroid CNB was greater in cases with suspicious US features [22,23]. In the present results, there were no cases of newly diagnosed malignancy in any of the 62 thyroid nodules. This discrepancy is due to differences in the inclusion criteria. The current study included CNB-proven benign thyroid nodules with previous inconclusive cytology. However, other studies have included thyroid nodules that simultaneously underwent FNA and CNB, US–pathology discordant nodules, or nodules with suspicious findings. Even though eight cases were K-TIRADS 5 on US, four cases were thyroiditis, and the condition nearly disappeared during follow-up. The other four cases were diagnosed as subcentimeter adenomatous hyperplasia based on the CNB results and remained stable without interval changes for >3 years.
This study had several limitations. First, nodules were evaluated in patients from a single center with a relatively small sample size. Only a small portion underwent surgical thyroid procedures. In cases of K-TIRADS 5 lesions with a subcentimeter size, the nodules were closely observed, without excision. Further investigation with a larger sample size and comprehensive surgical pathology will be required to better evaluate these patients. Second, the follow-up period was not enough to evaluate indolent thyroid cancer. As thyroid cancers can grow very slowly, this follow-up period may not have been sufficient to exclude slowly growing malignancies. Third, the outcomes of FNA versus CNB were not compared as repeated thyroid biopsy techniques for nodules with inconclusive cytology.
Although a portion of CNB-proven benign thyroid nodules showed changes in US features or nodule size during follow-up, these findings might simply represent a natural course of the nodules. Benign results for thyroid CNB after inconclusive FNA cytology might avoid unnecessary further management. However, a large series of multicenter studies would be needed to present a certain gold standard of follow-up for benign histology after CNB, especially in cases with a high level of suspicion based on the K-TIRADS category.
NotesAuthor Contributions Conceptualization: Hwang YJ, Park JS, Koo HR. Data acquisition: Hwang YJ, Park JS, Koo HR. Data analysis or interpretation: Park JS, Koo HR. Drafting of the manuscript: Hwang YJ, Park JS, Koo HR. Critical revision of the manuscript: Hwang YJ, Park JS, Koo HR. Approval of the final version of the manuscript: all authors. References1. Ha SM, Baek JH, Na DG, Jung CK, Suh CH, Shong YK, et al. Assessing the diagnostic performance of thyroid biopsy with recommendations for appropriate interpretation. Ultrasonography 2021;40:228–236.
2. Alexander EK, Heering JP, Benson CB, Frates MC, Doubilet PM, Cibas ES, et al. Assessment of nondiagnostic ultrasound-guided fine needle aspirations of thyroid nodules. J Clin Endocrinol Metab 2002;87:4924–4927.
3. Na DG, Kim JH, Sung JY, Baek JH, Jung KC, Lee H, et al. Coreneedle biopsy is more useful than repeat fine-needle aspiration in thyroid nodules read as nondiagnostic or atypia of undetermined significance by the Bethesda system for reporting thyroid cytopathology. Thyroid 2012;22:468–475.
4. Orija IB, Pineyro M, Biscotti C, Reddy SS, Hamrahian AH. Value of repeating a nondiagnostic thyroid fine-needle aspiration biopsy. Endocr Pract 2007;13:735–742.
5. Yang J, Schnadig V, Logrono R, Wasserman PG. Fine-needle aspiration of thyroid nodules: a study of 4703 patients with histologic and clinical correlations. Cancer 2007;111:306–315.
6. Yassa L, Cibas ES, Benson CB, Frates MC, Doubilet PM, Gawande AA, et al. Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer 2007;111:508–516.
7. Son HM, Kim JH, Kim SC, Yoo RE, Bae JM, Seo H, et al. Distribution and malignancy risk of six categories of the pathology reporting system for thyroid core-needle biopsy in 1,216 consecutive thyroid nodules. Ultrasonography 2020;39:159–165.
8. Na DG, Baek JH, Jung SL, Kim JH, Sung JY, Kim KS, et al. Core needle biopsy of the thyroid: 2016 consensus statement and recommendations from Korean Society of Thyroid Radiology. Korean J Radiol 2017;18:217–237.
9. Ha EJ, Chung SR, Na DG, Ahn HS, Chung J, Lee JY, et al. 2021 Korean Thyroid Imaging Reporting and Data System and imaging-based management of thyroid nodules: Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol 2021;22:2094–2123.
10. Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol 2016;17:370–395.
11. Jung CK, Min HS, Park HJ, Song DE, Kim JH, Park SY, et al. Pathology reporting of thyroid core needle biopsy: a proposal of the Korean Endocrine Pathology Thyroid Core Needle Biopsy Study Group. J Pathol Transl Med 2015;49:288–299.
12. Alexander EK, Hurwitz S, Heering JP, Benson CB, Frates MC, Doubilet PM, et al. Natural history of benign solid and cystic thyroid nodules. Ann Intern Med 2003;138:315–318.
13. Kuma K, Matsuzuka F, Yokozawa T, Miyauchi A, Sugawara M. Fate of untreated benign thyroid nodules: results of long-term follow-up. World J Surg 1994;18:495–498.
14. Lim DJ, Kim JY, Baek KH, Kim MK, Park WC, Lee JM, et al. Natural course of cytologically benign thyroid nodules: observation of ultrasonographic changes. Endocrinol Metab (Seoul) 2013;28:110–118.
15. Lee YJ, Kim JY, Na DG, Kim JH, Oh M, Kim DB, et al. Malignancy risk of thyroid nodules with minimal cystic changes: a multicenter retrospective study. Ultrasonography 2022;41:670–677.
16. Chernyavsky VS, Shanker BA, Davidov T, Crystal JS, Eng O, Ibrahim K, et al. Is one benign fine needle aspiration enough? Ann Surg Oncol 2012;19:1472–1476.
17. Ha EJ, Baek JH, Lee JH, Song DE, Kim JK, Shong YK, et al. Sonographically suspicious thyroid nodules with initially benign cytologic results: the role of a core needle biopsy. Thyroid 2013;23:703–708.
18. Hwang SH, Sung JM, Kim EK, Moon HJ, Kwak JY. Imaging-cytology correlation of thyroid nodules with initially benign cytology. Int J Endocrinol 2014;2014:491508.
19. Kim SY, Han KH, Moon HJ, Kwak JY, Chung WY, Kim EK. Thyroid nodules with benign findings at cytologic examination: results of long-term follow-up with US. Radiology 2014;271:272–281.
20. Kwak JY, Koo H, Youk JH, Kim MJ, Moon HJ, Son EJ, et al. Value of US correlation of a thyroid nodule with initially benign cytologic results. Radiology 2010;254:292–300.
21. Moon HJ, Kim EK, Yoon JH, Kwak JY. Malignancy risk stratification in thyroid nodules with nondiagnostic results at cytologic examination: combination of thyroid imaging reporting and data system and the Bethesda System. Radiology 2015;274:287–295.
22. Chung SR, Baek JH, Choi YJ, Sung TY, Song DE, Kim TY, et al. The role of core needle biopsy for the evaluation of thyroid nodules with suspicious ultrasound features. Korean J Radiol 2019;20:158–165.
23. Chung SR, Baek JH, Park HS, Choi YJ, Sung TY, Song DE, et al. Ultrasound-pathology discordant nodules on core-needle biopsy: malignancy risk and management strategy. Thyroid 2017;27:707–713.
24. Sung JY, Na DG, Kim KS, Yoo H, Lee H, Kim JH, et al. Diagnostic accuracy of fine-needle aspiration versus core-needle biopsy for the diagnosis of thyroid malignancy in a clinical cohort. Eur Radiol 2012;22:1564–1572.
Follow-up results of the nodules according to initial cytological reports.AUS, atypical cells of undetermined significance; FLUS, follicular lesions of undetermined significance; US, ultrasonography.
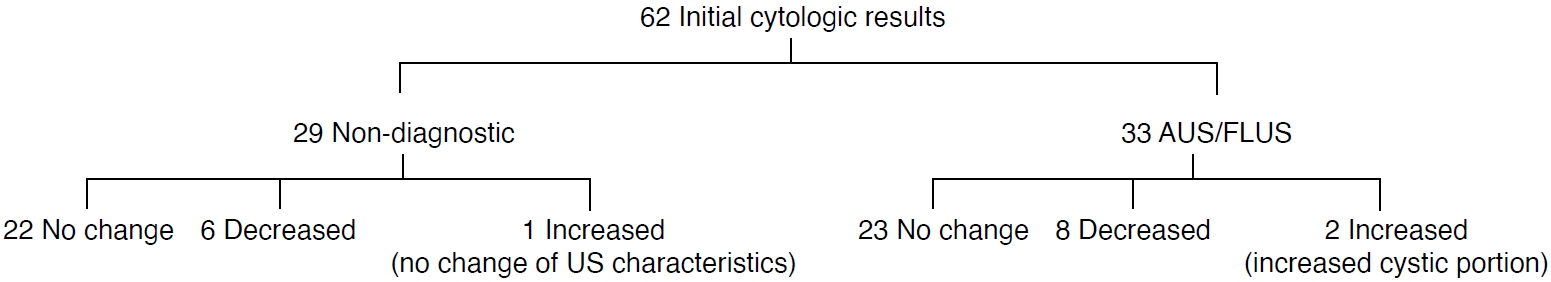 Fig. 1.A thyroid nodule showing interval growth after core needle biopsy.A. Longitudinal gray-scale ultrasonography (US) from a 43-year-old woman shows a solid and cystic, isoechoic, oval-shaped thyroid nodule. B. Longitudinal color Doppler US shows vascularity in the solid portion. Ethanol ablation was carried out. C. After 3 years, follow-up longitudinal US shows an increased nodule size with an increased cystic portion. D. Re-core needle biopsy reveals a benign follicular nodule.
 Fig. 2.A thyroid nodule that disappeared during ultrasonography (US) follow-up.A, B. Transverse (A) and longitudinal (B) gray-scale US from a 48-year-old woman show a taller-than-wider, hypoechoic, ill-defined thyroid nodule. Core needle biopsy reveals chronic lymphocytic thyroiditis. C. Follow-up longitudinal US shows normalization of the thyroid parenchyma after 1 year.
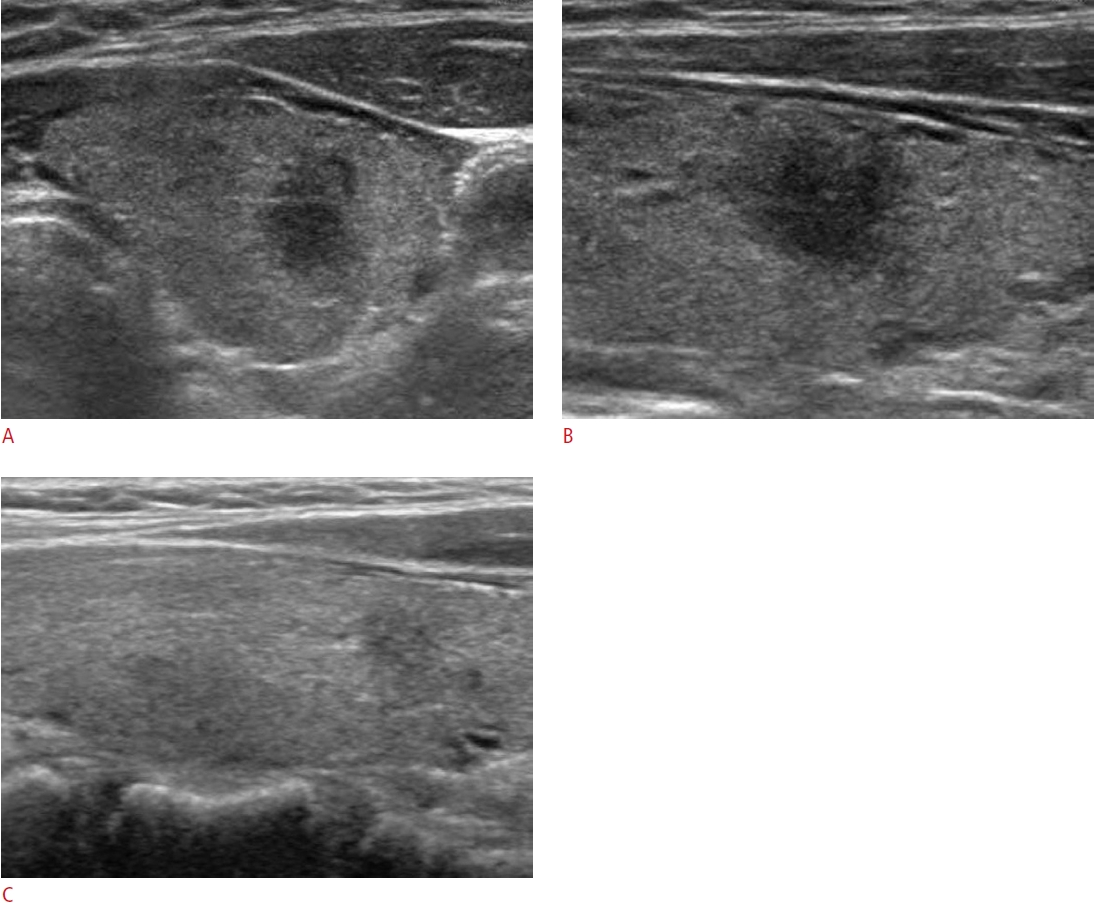 Fig. 3.Table 1.Baseline demographics of the study population Table 2.Ultrasonographic findings of thyroid nodules with benign histology Table 3.The characteristics of CNB-confirmed benign thyroid nodules with K-TIRADS 5 on ultrasonography
Table 4.The characteristics of CNB-proven benign thyroid nodules with interval growth
Table 5.Summary of malignancy rates in cases with benign histology on thyroid CNB in previously published studies
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||



 Print
Print facebook
facebook twitter
twitter Linkedin
Linkedin google+
google+
 Download Citation
Download Citation PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI




