A preliminary study of shear-wave elastography for the evaluation of varicocele in adolescents and young adults
Article information
Abstract
Purpose
The purpose of this study was to use shear-wave elastography (SWE) to assess testicular stiffness changes during the Valsalva maneuver in adolescents and young adults with varicocele, to compare these changes according to clinical severity, and to evaluate the role of SWE in the diagnosis of varicocele.
Methods
This study included patients undergoing testicular ultrasonography for the diagnosis of varicocele or for post-varicocelectomy follow-up between June 2016 and February 2017. Fifty-four testicles of 27 consecutive patients (mean age, 15.9 years) were classified by clinical grade (grade 0-3). Using SWE, mean testicular stiffness (Emean) was measured at rest and during the Valsalva maneuver. The correlations between multiple ultrasonographic parameters (volume asymmetry, Emean at rest, and absolute and percentage changes in Emean during the Valsalva maneuver) and clinical grade were assessed using the Spearman correlation test.
Results
The Emean at rest was similar across clinical grades. During the Valsalva maneuver, increased testicular stiffness was frequently observed in patients with grade 2 or 3 varicocele but rarely observed in those with grade 0 or 1 varicocele. The changes in Emean were positively correlated with the clinical grade (all P<0.001), whereas the Emean at rest and volume asymmetry were not (all P>0.05).
Conclusion
A transient, reversible increase in testicular stiffness during the Valsalva maneuver was observed in adolescents with high-grade varicocele, and the degree of stiffness change was correlated with the clinical grade. Stiffness change identified using SWE during the Valsalva maneuver is a potential surrogate indicator of venous congestion.
Introduction
Varicocele is a major cause of male secondary infertility and is associated with abnormal semen characteristics such as sperm dysmotility and decreased sperm count, testicular atrophy, and changes in Leydig and Sertoli cell function [1]. In addition, varicocele has a progressive long-term detrimental effect on spermatogenesis, especially in adolescents. Therefore, it is essential to perform accurate, reliable, and regular follow-up assessments and to determine a treatment plan and surgical timing.
As ultrasonography (US) is a widely used modality for diagnosing varicocele, several severity grading systems based on grayscale US and Doppler US have been proposed for objective and consistent evaluation [2,3]. However, these grading systems have limited clinical relevance because they exhibit a low correlation with abnormal semen parameters that reflect impaired spermatogenesis. Additionally, they consider only the degree and extent of dilated spermatic veins rather than the changes in the testicular parenchyma itself [4].
Recently, several sonoelastographic methods that provide information about the stiffness of tissues have been introduced to evaluate microenvironmental parenchymal changes in solid organs. Among the sonoelastography techniques, shear-wave elastography (SWE) is a novel, reproducible, and noninvasive method that provides quantitative data for the assessment of parenchymal diseases affecting solid organs such as the testis, liver, kidney, and thyroid gland. The diagnostic usefulness of testicular sonoelastography has been investigated in studies of undescended testis, testicular microlithiasis, scrotal hydrocele, testicular torsion, and malignant tumors [5-9]. In several previous studies, varicocele was found to change the testicular stiffness as measured by elastography [10-13]. In addition, those studies indicated that sonoelastography may predict the improvement of abnormal semen parameters after varicocelectomy as well as that of significant volume difference and infertility related to abnormal semen characteristics such as decreased sperm count [10-13]. However, in these previous studies, the stiffness was examined only at the resting state. Given that the Valsalva maneuver is an essential process for assessing the clinical severity of varicocele during a physical examination, a study of stiffness changes caused by the Valsalva maneuver could be useful for diagnosing varicose veins and understanding the pathophysiology of varicocele. Therefore, the purpose of this study was to use SWE to assess the change in testicular stiffness during the Valsalva maneuver in adolescents and young adults with varicocele, to compare these changes according to clinical severity, and to evaluate the role of SWE in the diagnosis of varicocele.
Materials and Methods
Compliance with Ethical Standards
This retrospective study was approved by the institutional review board of Seoul National University Hospital (IRB No. 2105-075-121), and the requirement for informed consent was waived.
Patients
All patients undergoing testicular US for the diagnosis of varicocele or for follow-up after varicocelectomy between June 2016 and February 2017 at the authors’ institution were included in this study. A total of 54 testicles of 27 consecutive patients (mean age, 15.9 years; range, 12 to 20 years) were enrolled and assessed by pediatric urologists according to the clinical grading system established by Dubin and Amelar [14]. On the basis of physical examination, varicoceles were graded as follows: grade 0 (normal or subclinical), not palpable or visible at rest or during the Valsalva maneuver; grade 1, palpable during the Valsalva maneuver but not otherwise; grade 2, palpable at rest but not visible; and grade 3, palpable and visible at rest.
Among the 54 testicles of the enrolled patients, 27 testicles were categorized as normal or subclinical (grade 0), six testicles as grade 1, eight testicles as grade 2, and 13 testicles as grade 3 varicocele, respectively. Three patients had bilateral varicoceles, three patients had no varicocele, and the remaining 21 patients had a unilateral left varicocele. All three patients with bilateral varicoceles had a higher grade on the left side than on the right side. In all three patients with bilateral varicoceles, the clinical grade was 1 in the right testis and 2 or 3 in the left testis.
Six of the 27 patients were enrolled in the study after varicocelectomy. Five patients had undergone left varicocelectomy, and the other patient had undergone bilateral varicocelectomy. Of the seven testes that were followed up on after surgery, three were classified as normal or subclinical, one as grade 1, two as grade 2, and one as grade 3 varicocele.
Ultrasonography and SWE
The patients underwent grayscale US and SWE with a 15-4-MHz linear-array transducer using an Aixplorer ultrasound system (Supersonic Imagine, Aix-en-Provence, France). All US images were obtained by an experienced pediatric radiologist (Y.H.C., who had 16 years of clinical experience). The testicular volume was measured three-dimensionally and calculated using the following formula: testicular volume=length×width×height×0.523.
In SWE, tissue elasticity was visualized using a color-coded map representing the Young modulus in kilopascals (kPa) at each pixel in the range from blue (soft) to red (hard), and the scale range was set at 0-10 kPa. Testicular stiffness was measured under two respiratory conditions: at rest and during the Valsalva maneuver. The region of interest (ROI) was set at the center of the testicle, and the ROI diameter was 9-11 mm. The operator attempted to draw the ROIs for the two conditions as close to each other as possible (Supplementary Fig. 1). The mediastinum testis was excluded from the ROIs. By setting the ROI, several quantitative elasticity values were obtained from the system, including mean stiffness (Emean). As in previously published studies regarding testicular SWE, automatically-generated mean stiffness was used instead of the median value [5,6,9]. Stiffness was measured one to three times, and the average of the Emean was used for the analyses.
Statistical analysis was conducted using several calculated parameters, including testicular volume asymmetry, the change in stiffness during the Valsalva maneuver, and the percentage (or relative) change in stiffness during the Valsalva maneuver. These parameters were calculated using the following formulas:
Volume asymmetry (%)= (right testicular volume-left testicular volume)/right testicular volume×100
Absolute change in stiffness (kPa)=stiffness during the Valsalva maneuve-stiffness at rest
Percentage change in stiffness (%)= (stiffness during the Valsalva maneuver-stiffness at rest)/stiffness at rest×100
The volume asymmetry was calculated only in cases of preoperative left unilateral varicocele (n=18).
Statistical Analysis
The correlation between each US parameter (volume asymmetry, Emean at rest, Emean during the Valsalva maneuver, and absolute and percentage changes in Emean during the Valsalva maneuver) and clinical grade was assessed using the Spearman correlation test. For parameters that showed a statistically significant correlation, a linear mixed-model within-subject analysis was performed to determine the strength of the association found between the parameter and the study variables, while controlling for clustering effects caused by multiple measurements taken in the same patients.
All statistical analyses were performed with SPSS software version 25.0 (IBM Corp., Armonk, NY, USA), and P-values <0.05 were considered to indicate statistical significance.
Results
Table 1 demonstrates the volume asymmetry and stiffness of the testicles at rest and during the Valsalva maneuver according to the clinical grade. The stiffness was measured using SWE for all 54 testicles. The Emean measured at the resting state was similar among the four clinical grades. However, the Emean during the Valsalva maneuver, the change in Emean, and the percentage change in Emean during the Valsalva maneuver gradually increased with increasing clinical grade (Figs. 1, 2, Video clips 1, 2). Grades 0 and 1 exhibited similarly low values, grade 2 exhibited a slightly higher value, and grade 3 displayed the highest value.

Elastographic and conventional ultrasonographic parameters of grade 0, 1, 2, and 3 testicular varicoceles

A 13-year-old boy with grade 3 left unilateral varicocele.
Shear-wave elastography and corresponding grayscale ultrasonographic images of the left testicle (A) and right testicle (B) at rest (left column) and during the Valsalva maneuver (right column) are shown. The images show increased stiffness of the left testicle after the Valsalva maneuver compared with the stiffness at rest (absolute change in Emean, 0.9 kPa; percentage change in Emean, 34.6%), while no significant change was observed in the stiffness of the right testicle between the two conditions (absolute change in Emean, 0.03 kPa; percentage change in Emean, 1.2%). Emean, mean stiffness.

A 14-year-old boy with grade 3 left unilateral varicocele.
Shear-wave elastography ultrasonographic images of the left testicle (A) and the right testicle (B) at rest (left column) and during the Valsalva maneuver (right column) are shown. The images show increased stiffness of the left testicle after the Valsalva maneuver compared with the stiffness at rest (absolute change in Emean, 0.5 kPa; percentage change in Emean, 21.7%), while no significant change was observed in the stiffness of the right testicle between the two conditions (absolute change in Emean, 0.1 kPa; percentage change in Emean, 4.5%). Emean, mean stiffness.
A positive correlation was found between clinical grade and the Emean during the Valsalva maneuver, as well as between clinical grade and the change of stiffness between the two conditions (Emean during the Valsalva maneuver, ρ=0.399, P=0.003; absolute change in Emean during the Valsalva maneuver, ρ=0.597, P<0.001; percentage change in Emean during the Valsalva maneuver, ρ=0.574, P<0.001). However, the clinical grade did not show a significant association with volume asymmetry or the Emean at rest (volume asymmetry, ρ=-0.110, P=0.664; Emean at rest, ρ=0.098, P=0.483).
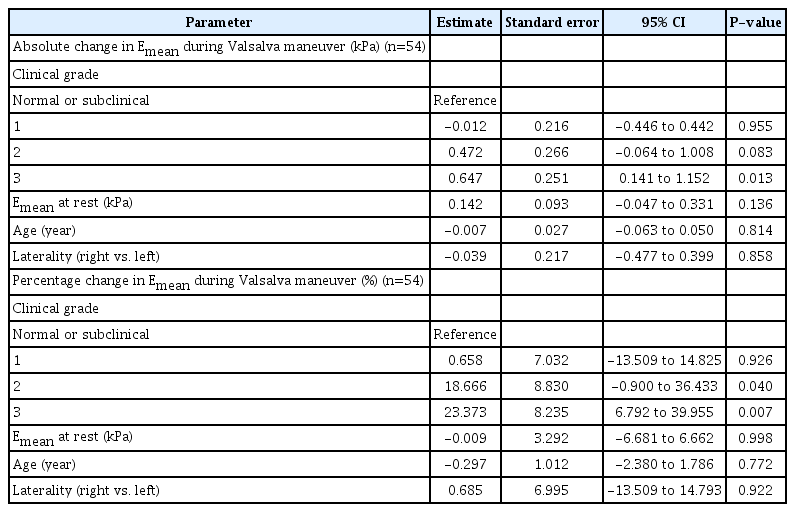
A linear mixed-model within-subject analysis including the 54 testes of the 27 patients was performed with the absolute and percentage changes in Emean during the Valsalva maneuver as the dependent outcomes. The clinical grade of varicocele, Emean at rest, patient age, and laterality of the testes were considered fixed effects, and the patients were considered random effects. In the linear mixed-model analyses, the clinical grade showed a statistically significant, positive effect on the absolute and percentage changes in Emean during the Valsalva maneuver (Table 2). The absolute change in Emean during the Valsalva maneuver was significantly higher in grade 3 cases than in grade 0 or 1 cases (P=0.013 and P=0.010, respectively) (Supplementary Table 1). In addition, the percentage changes in Emean during the Valsalva maneuver in grade 2 and 3 cases were significantly higher than those in grade 0 and 1 cases (all P<0.05) (Supplementary Table 1). Statistically significant differences in the absolute and percentage changes in Emean during the Valsalva maneuver were not observed between grades 0 and 1 or between grades 2 and 3. In contrast, the Emean at rest, patient age, and laterality of the testes showed no significant effects on the absolute and percentage changes in Emean (all P>0.05).
A significant increase in stiffness during the Valsalva maneuver was defined as a change above the average of Emean in grade 0 testicles plus twice the standard deviation. The number and proportion of testicles with significant increases were analyzed for each clinical grade. At the cutoff value of 0.50 kPa for the absolute change in Emean, the proportion of testicles that exhibited significantly increased stiffness was 3.7% (one of 27) in grade 0, 0% (0 of six) in grade 1, 37.5% (three of eight) in grade 2, and 53.8% (seven of 13) in grade 3 cases. At the cutoff value of 17.9% for the percentage change in Emean, the proportion of testicles with significantly increased stiffness was 3.7% (one of 27) in grade 0, 0% (0 of six) in grade 1, 50% (four of eight) in grade 2, and 61.5% (eight of 13) in grade 3 cases. For both the absolute and percentage changes in Emean, grade 3 cases thus had the highest proportion of significant changes, followed by cases in grades 2, 0, and 1 (Fig. 3).

Absolute (A) and percentage (B) changes in mean testicular stiffness during the Valsalva maneuver according to clinical grade.
Dotted lines indicate averages of mean stiffness of grade 0 testicles plus twice the standard deviation, and the cutoff values are 0.50 kPa in (A) and 17.9% in (B). Emean, mean stiffness.
Discussion
Understanding the microenvironmental alterations caused by varicocele in the testicular parenchyma is crucial in the prediction of prognosis and treatment planning. In addition, objective and quantitative evaluations of the affected testis would enable clinicians to monitor disease progression, determine the effect of surgical intervention, detect recurrence early, and assess the need for reoperation. In this preliminary study, increased testicular stiffness during the Valsalva maneuver was frequently observed in patients with high-grade varicoceles, while it was rarely observed in those with low-grade varicoceles, regardless of the stiffness at rest. All but one patient with an absolute stiffness increase of >0.5 kPa presented with grade 2 or 3 varicocele. In contrast, other US parameters, including testicular volume asymmetry and testicular stiffness at rest, were not associated with the clinical severity of varicocele.
All previous studies on the elastographic evaluation of varicocele involved measurements of testicular stiffness at rest. These studies showed a persistent increase in the stiffness of testicles with varicoceles [10-12]. In particular, Camoglio et al. [10] found that varicocele increased the testicular stiffness, which was positively correlated with the clinical grade and the duration of spermatic vein reflux. The authors assumed that chronic varicocele leads to increased deposition of interstitial fibrous tissue and that these fibrous changes in testicular tissue can aggravate testicular stiffness, testicular hypotrophy, and impaired spermatogenesis [15]. However, the result of the present study differs from those of previous studies in that testicular stiffness at rest did not significantly differ among the clinical grades. This could be attributed to the relatively young study population in the present study; all 27 patients were adolescents (mean age, 15.9 years; range, 12 to 20 years). Therefore, the findings may be explained by the younger age of the patient population without chronic fibrosis.
Interestingly, this young study population showed no increase in testicular stiffness at rest, whereas a transient and reversible increase of testicular stiffness during the Valsalva maneuver was observed in some patients with varicocele. Furthermore, the degree of stiffness increase during the Valsalva maneuver was correlated with the clinical grade. This can be explained by the fact that the Valsalva maneuver can lead to venous congestion due to venous reflux, resulting in increased stiffness in the testicles with varicoceles. As increased venous pressure is one proposed mechanism for the pathophysiology of varicocele-induced infertility, congestion of the testicular parenchyma as measured by SWE could be an important imaging marker for predicting prognosis [16].
Calculating the difference between the stiffness value measured during normal breathing and that measured during the Valsalva maneuver has another advantage over simply utilizing the absolute stiffness value during normal breathing. In particular, a single measurement of SWE under a certain condition (such as normal breathing) may have limited utility in the diagnosis of adolescent varicocele because testicular stiffness tends to decrease as the testicular volume increases during normal growth [17]. A dynamic provocation test could be more helpful than a static test in diagnosing varicocele, and SWE measurements during both normal breathing and the Valsalva maneuver may be useful for evaluating varicocele in adolescents.
Approximately half of the testicles with clinical grade 2 or 3 varicocele exhibited significantly increased stiffness during the Valsalva maneuver, compared to one testis classified as grade 0. These results imply that the severity of testicular parenchymal congestion may show individual variations even among cases of the same clinical grade. A comparative analysis of clinical grade and SWE changes, which are more closely related to prognosis, is needed in future studies investigating clinical and histologic features and semen test results.
In this study, conventional grayscale US parameters, including volume asymmetry, were not found to be associated with the severity of varicocele. The combination of testicular asymmetry greater than 20% and peak retrograde flow velocity above 38 cm/s has been demonstrated in many studies as a promising indicator of progressive testicular atrophy in adolescents with varicocele [18-20]. However, as noted in this study, these parameters are not valid for all patients; additionally, it is difficult to obtain the parameters adequately, and considerable inter-observer and inter-institutional variabilities exist [21-23]. Additionally, volume asymmetry alone should not be used as a surgical indicator because asymmetric growth in normal puberty and catch-up growth in patients with varicocele can cause temporary volume asymmetry [24-26].
In this study, stiffness was compared across clinical grades because of the current realities of clinical practice. A physical examination-based classification system is still considered a mainstay and the gold standard in diagnosing clinically significant varicocele, despite the intrinsic limits of subjective assessments [4,21-23]. As mentioned previously, many US-based classification systems have emerged to replace the clinical grading system; however, they have not been accepted as gold-standard methods owing to their limited clinical utility.
In addition to diagnosis, an important role of ultrasonography in varicocele is to provide prognostic information. SWE could provide such crucial information. The present study demonstrated a correlation between testicular stiffness changes during the Valsalva maneuver and the degree of clinical severity. This correlation could indicate the potential of SWE to provide prognostic information. Interestingly, only a portion of patients with grades 2 or 3 varicocele exhibited significant changes in testicular stiffness during the Valsalva maneuver. It is worth wondering whether any difference in prognosis will exist between patients with and without significant stiffness changes. Theoretically, stiffness reflects the testicular parenchymal pressure; therefore, stiffness changes could provide better prognostic information than a simple clinical grading system. To support this theory, further studies assessing correlations of SWE findings with the degree of testicular atrophy, semen parameters, and fertility are required.
This study had several limitations in addition to those inherent to all retrospective studies. First, the number of enrolled patients was small. Second, normal controls were not included for comparison. Third, it was not possible to correlate semen analysis with the SWE results because most of the patients included in this study were adolescents, and the institution at which this study was conducted does not perform semen analysis in this age group. Fourth, follow-up SWE measurement was not performed after varicocelectomy. Fifth, variability in the number of measurements may lead to variability of the stiffness in the study results. However, according to a previous study, three SWE measurements can be sufficient to assess hepatic stiffness in children 6 years of age and older [27]. Moreover, unlike the liver, the testicles are not moved by breathing and are positioned superficially; thus, it is thought that less variability exists and that good-quality values can be obtained even with fewer than three measurements. Sixth, it was not possible to assess interobserver variation in this study because a single operator performed SWE ultrasonography and measured the stiffness. Seventh, during the Valsalva maneuver, the patients’ compliance can affect the change in stiffness.
In conclusion, a transient and reversible increase of testicular stiffness during the Valsalva maneuver was observed in adolescents with high-grade varicocele, and the degree of stiffness change was correlated with the clinical grade. SWE evaluation of the testes in adolescents with varicocele is a feasible noninvasive imaging modality, and SWE changes during the Valsalva maneuver could be used as a surrogate indicator of venous congestion.
Notes
Author Contributions
Conceptualization: Ryu YJ, Choi YH, Cheon JE, Kim WS, Kim IO. Data acquisition: Ryu YJ, Choi YH, Park JE. Data analysis or interpretation: Ryu YJ, Choi YH, Kim JY, Im YJ, Park K. Drafting of the manuscript: Ryu YJ, Choi YH. Critical revision of the manuscript: Ryu YJ, Choi YH, Kim JY, Cheon JE, Kim WS, Kim IO, Park JE, Im YJ, Park K. Approval of the final version of the manuscript: all authors.
Jung-Eun Cheon serves as Editor for the Ultrasonography, but has no role in the decision to publish this article. All remaining authors have declared no conflicts of interest.
Supplementary Material
Supplementary Table 1.
Results of the post-hoc test in the linear mixed-model analysis (https://doi.org/10.14366/usg.20213)
Supplementary Fig. 1.
Quantification of the testicular stiffness using shear wave elastography (SWE) in a 13-year-old boy. A color-coded SWE map displaying a spectrum of colors for the related SWE values is generated. If the testicular bordes is not clear, the SWE map and synchronized B-mode-ultrasonographic image are displayed together up and down. A 10 mm diameter circular region of interest (ROI) is drawn in the center of the testis and the mediastinum testis is excluded from the ROI. By setting ROI, several quantitative elasticity values are obtained from the system including the mean stiffness (https://doi.org/10.14366/usg.20213).
Video clip 1.
Shear-wave elastography sonogram of the left testicle of a 14-year-old boy with grade 3 left unilateral varicocele during the Valsalva maneuver (same patient as in Fig. 2) (https://doi.org/10.14366/usg.20213.v001).
Video clip 2.
Shear-wave elastography sonogram of the right testicle of a 14-year-old boy with grade 3 left unilateral varicocele during the Valsalva maneuver (same patient as in Fig. 2) (https://doi.org/10.14366/usg.20213.v002).
References
Article information Continued
Notes
Key point
A transient and reversible increase in testicular stiffness can be observed during Valsalva maneuver in adolescents with varicocele. The more severe the varicocele, the more frequent and greater the changes in testicular stiffness.