Benign core biopsy of probably benign breast lesions 2 cm or larger: correlation with excisional biopsy and long-term follow-up
Article information
Abstract
Purpose:
To evaluate the accuracy of benign core biopsy of probably benign breast lesions (category 3) 2 cm or larger on the basis of excisional biopsy and long-term follow-up.
Methods:
We retrospectively reviewed 146 category 3 lesions in 146 patients 2 cm or larger which were diagnosed as benign by ultrasound (US)-guided core biopsy. Patients were initially diagnosed as benign at core needle biopsy and then followed up with excisional biopsy (surgical excision, n=91; US-guided vacuum assisted excision, n=35) or breast ultrasonography (n=20).
Results:
Of the 126 patients who underwent surgical excision or US-guided vacuum-assisted excision, 114 patients were diagnosed with benign lesions, 10 patients with borderline lesions (benign phyllodes tumor), and two patients with malignant phyllodes tumors. The probabilities of lesions being benign, borderline and malignant were 91.8% (134/146), 6.8% (10/146), and 1.4% (2/146), respectively. Of 13 patients who had growing masses on follow-up ultrasonography, three (23.1%) were non-benign (two benign phyllodes tumors and one malignant phyllodes tumor).
Conclusion:
US-guided core needle biopsy of probably benign breast mass 2 cm or larger was accurate (98.6%) enough to rule out malignancy. But, it was difficult to rule out borderline lesions even when they were diagnosed as benign.
Introduction
High resolution breast ultrasonography has been increasingly used because of its advantages in the detection, characterization and differentiation of lesions, with lesions being diagnosed as benign to malignant [1-3]. According to the Breast Imaging-Reporting and Data System (BI-RADS), category 3, probably benign, on ultrasonography is defined as a solid mass with oval shape, circumscribed margin, parallel orientation, and no suspicious malignant features [4]. Short-interval follow-up is most often recommended for category 3 lesions because the probability of malignancy is low (<2%) and unnecessary breast biopsies of benign lesions, morbidity and medical costs can all be reduced with just follow-up.
Even though palpable or non-palpable probably benign lesions have a short-interval imaging follow-up recommended rather than biopsy, the triple test (physical examination, mammogram, and fineneedle aspiration) or modified triple test (physical examination, mammography and/or ultrasonography, and fine-needle aspiration and/or biopsy) has been used to evaluate palpable lesions in clinical practice [5]. However, there is relatively little research on the accuracy of core needle biopsy for palpable lesions [6-9] and, in particular, on its ability to identify borderline lesions.
The purpose of our study was to investigate the accuracy of benign core needle biopsy of probably benign breast masses 2 cm or larger on the basis of excisional biopsy and long-term follow-up.
Materials and Methods
Institutional Review Board approval was obtained for this retrospective study.
Study Population
We retrospectively reviewed lesions assessed as category 3 probably benign according to BI-RADS from October 2001 to December 2009. Among 207 patients who were initially assessed with category 3 solid masses 2 cm or larger on ultrasonography with US-guided core needle biopsy (US-CNB), 199 patients were diagnosed with benign lesions and the remaining 8 patients were diagnosed with malignant (n=1, invasive ductal carcinoma) or borderline lesions (n=7; 6 phyllodes tumors, 1 intraductal papilloma). Among 199 patients with benign biopsies, 53 patients were excluded because they were lost to follow-up less that was than 2 years. Finally, 146 masses in 146 patients were included in this study (Fig. 1).

Flow chart of the study population.
US, ultrasound; US-VAE, ultrasound-guided vacuum-assisted excision.
Pathologic results of US-CNB were as follows: fibroadenoma (n=64), fibrocystic change (n=25), stromal fibrosis (n=18), fibroadenomatous hyperplasia (n=19), adenosis (n=4), benign breast tissue such as fibroadipose tissue (n=5), duct ectasia (n=4), apocrine metaplasia (n=1), ductal epithelial hyperplasia (n=1), granular cell tumor (n=1), lactating adenoma (n=1), lactating adenosis (n=1), palisading granuloma (n=1), and sclerosing adenosis (n=1).
Ultrasonography and US-guided Core Needle Biopsy
Ultrasonography was performed using a 5-10 MHz or 5-12 MHz linear array transducer (HDI 3000 or 5000, Advanced Technology Laboratories, Philips Medical Systems, Bothell, WA, USA; Logic 9, GE Healthcare, Milwaukee, WI, USA; iU22, Philips Healthcare, Bothell) by one of nine dedicated breast imaging radiologists with 1 to 11 years of experience. All ultrasonography examinations included bilateral whole-breast imaging and were classified into one of five final assessments according to the BI-RADS lexicon. Category 3 probably benign was defined as a solid mass with oval shape, circumscribed margin, parallel orientation, and no suspicious malignant features. After ultrasonography, US-CNB was performed using a 14-gauge automated core needle and a spring-loaded biopsy gun (Promac 2.2L, Manan Medical Products, Northbrook, IL, USA). Local anesthesia was routinely applied and at least 5 core samples were obtained.
Follow-up Ultrasonography
After each biopsy, follow-up ultrasonography was recommended at 6 months, 12 months, and 24 months. At follow-up ultrasonography, a lesion-to-lesion comparison was performed. If a lesion showed no change in size and characteristics over 24 months, the final assessment was changed to category 2 benign. However, if a lesion increased in size in more than 10% of its initial maximal diameter or showed any changes in its characteristics on follow-up ultrasonography, the lesion was upgraded to category 4 or 5 and US-CNB was recommended [10-12].
Surgical Excision or US-guided Vacuum-assisted Excision
Depending on patients’ or physicians’ preference, surgical excision or US-guided vacuum-assisted excision (US-VAE) was performed. US-VAE using an 8-gauge needle (Mammotome, Ethicon Endo- Surgery, Cincinnati, OH, USA) was performed as described by Kim et al. [13]. To ensure complete mass removal during VAE, we removed breast tissue surrounding the lesion at approximately four more sampling sites (12, 3, 6, and 9 o’clock directions).
Reference Standards
Among a total of 146 masses, 91 masses underwent surgical excision, 35 masses US-VAE, and 20 masses follow-up ultrasonography. Surgical excision or US-VAE was considered to be the gold standard for most lesions. For lesions without changes over two years of follow-up ultrasonography, follow-up ultrasonography alone was considered to be the gold standard. On the basis of pathologic results and follow-up ultrasonography, we calculated the probabilities of lesions being benign, borderline and malignant. Borderline pathologies included benign or borderline phyllodes tumor.
Statistical Analysis
Statistical analyses were performed using IBM SPSS ver. 19.0 (IBM Co., Armark, NY, USA). P<0.05 was considered to indicate statistical significance. One-way ANOVA was used to compare age and size on follow-up modalities. The independent t-test was used to compare age and size on final pathology. The chi-square test was used to compare presence of symptoms and diameter changes on final pathology.
Results
All 146 patients in this study were women and 124 patients complained of palpable masses. The mean age of the patients was 35.7 years, ranging from 13 to 72 years. The mean size of the masses was 31.8 cm with a range of 2.0-12 cm.
Correlation with Gold Standards
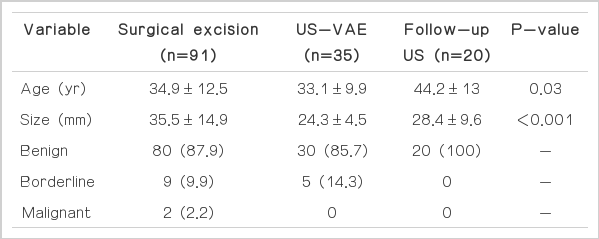
Among the total 146 masses, surgical excision was done in 91 masses, US-VAE in 35 masses and follow-up in 20 masses (Table 1). Patients who underwent surgical excision were older and had larger mass size (P<0.05) than other follow-up modalities. The mean interval between initial US-CNB and surgical excision or US-VAE was 129.7 days (range, 1 to 1,976 days) and 215 days (range, 6 to 1,621 days), respectively. A total of 20 masses in 20 patients were followed with ultrasonography only with a mean follow-up interval of 1,664.9 days (range, 897 to 3,027 days). All 20 masses were stable or decreased in size after US-CNB over 2 years of follow-up ultrasonography.
Finally, 134 patients were diagnosed with benign lesions (Fig. 2), two patients were diagnosed with malignancies which were all malignant phyllodes tumors (Fig. 3), and 10 patients were diagnosed with borderline lesions. So, the probabilities of lesions being benign, borderline, and malignant were 91.8% (134/146), 6.8% (10/146), and 1.4% (2/146), respectively.
A 36-year-old woman with a palpable mass in her left breast.
Transverse (A) and longitudinal (B) ultrasonography reveal a circumscribed, oval, hypoechoic mass in the left lower inner breast. The initial diameter of the mass was 20×13×19 mm and the pathologic result of ultrasound-guided core needle biopsy was fibroadenoma. The patient underwent surgical excision 82 days later and the result was fibroadenoma.
A 28-year-old woman with a mass in her left breast.
Transverse (A) and longitudinal (B) ultrasonography reveal a circumscribed, oval, hypoechoic mass in the left upper outer breast. The initial diameter of the mass was 53×26×50 mm and the pathologic result of ultrasound-guided core needle biopsy was fibroadenomatous hyperplasia. The patient underwent surgical excision 21 days later and the result was malignant phyllodes tumor.
Comparison of Benign and Non-Benign Lesions
Table 2 compares the characteristics of the benign and non-benign groups. Age, size, and presence of symptoms were not statistically different between the benign and non-benign lesions. Among 126 lesions in which surgical excision and US-VAE were performed, 13 cases (10.3%) showed the maximal diameter increased by more than 10% of its initial maximal diameter (Fig. 4). The pathologic results of 13 growing masses were malignant phyllodes tumor (n=1), benign phyllodes tumor (n=2), fibroadenoma (n=5), fibrocystic change (n=2), fibroadenomatous hyperplasia (n=2), and sclerosing adenosis (n=1).

A 42-year-old woman with a palpable mass in her left breast.
A. Transverse ultrasonography reveals a circumscribed, oval, hypoechoic mass in the left upper center breast. The initial diameter of the mass was 17×43 mm and the pathologic result of ultrasound-guided core needle biopsy was fibrocystic change. B. Longitudinal ultrasonography reveals that the lesion shows an interval increase in diameter, measuring 26×76 mm after 54 months. The patient underwent surgical excision and the result was stromal fibrosis and sclerosing adenosis.
Discussion
Ultrasonography has been increasingly used and is an important adjunct to mammography in the diagnosis of breast diseases [14]. In 2003, ACR developed a BI-RADS ultrasonography lexicon and a category 3 probably benign lesion is defined as a solid mass with oval shape, circumscribed margin, parallel orientation, and no suspicious malignant features [4]. It is not a definite benign designation but is expected to be changed infrequently [15].
Several early studies supported the rationale that probably benign lesions could be just followed up because of their low risk of malignancy (<2%) [10-12,16]. Other recent studies also reported similar results which concluded that category 3 probably benign lesions should be recommended for follow-up rather than immediate biopsy [17-19]. However, further diagnostic imaging work-up should be preceded before assessing a lesion as probably benign and recommending follow-up [11,20,21]. During follow-up, the initial follow-up at 6 months is the most important evaluation because rapidly growing cancer can be detected without delay [15]. However, less than 2% of probably benign lesions are diagnosed as malignancy at this point. Leung and Sickles [22] in their cohort study of 1,440 multiple-mass cases reported that the interval cancer rate (0.14%) was lower than the age-matched United States incident cancer rate (0.24%).
Among a total of 146 masses in this study, surgical excision was done in 91 masses, US-VAE in 35 masses and follow-up in 20 masses. Patients who underwent surgical excision were older and had larger mass size (P<0.05) than other follow-up modalities. Of 146 masses, 134 masses were diagnosed as benign, 10 masses were borderline lesions and two were malignancy. The probabilities of a lesion being benign, borderline and malignant were 91.8% (134/146), 6.8% (10/146), and 1.4% (2/146), respectively. Of the two malignancies, one showed interval growth on follow-up ultrasonography.
According to the BI-RADS lexicon, a newly detected lesion or an enlarged lesion on follow-up mammogram should undergo prompt biopsy [4]. Varas et al. [10] reported that when probably benign lesions showed an increase in size, loss of distinct borders, increase in the number of microcalcifications, new forms of calcifications, newly appeared mass within microcalcifications and palpable lumps, prompt biopsy was recommended even if it had been previously assessed as probably benign. Recently several reports demonstrated that probably benign lesions with interval growth should unde biopsy or excision [23-26]. Moon et al. [23] recommended prompt biopsy if probably benign lesions showed changes in lesion characteristics as well as interval growth on follow-up ultrasonography because the malignancy rate increased to 38.5%. In our study, a total of 13 masses showed interval growth on followup ultrasonography and one was malignant (7.7%, 1/13). Therefore, further study such as surgery, US-VAE or US-CNB is recommended when probably benign lesions show interval growth even if initial biopsy results are benign.
In this study, surgically confirmed phyllodes tumor were regarded as borderline lesions because the management and behavior of benign phyllodes are different with fibroadenoma. Phyllodes tumor should be treated by wide surgical excision with clear margin whereas fibroadenoma is effectively managed by simple enucleation [27]. Also it has a tendency to recur, metastasize regardless of its histology and malignant potential in some of cases [28,29]. Therefore, we considered and analyzed benign phyllodes tumor as borderline lesion.
There were several limitations in this study. First, this study was a retrospective study with a relatively small number of patients. Second, ultrasonography is an operator-dependent process and there may be measurement variability among radiologists who perform ultrasonography.
In conclusion, US-CNB of probably benign breast lesions with benign biopsy results 2 cm or larger was accurate (98.6%) enough to rule out malignancy. But, it was difficult to rule out borderline lesions even after they were diagnosed as benign through US-CNB.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported in part by the Research Fund of the Korean Society of Ultrasound in Medicine.