AbstractPurposeThis study investigated the clinical and ultrasonographic (US) findings of suture granulomas and recurrent tumors, and aimed to identify specific characteristics of suture granulomas through an experimental study.
MethodsThis retrospective study included 20 pathologically confirmed suture granulomas and 40 recurrent tumors between January 2010 and December 2020. The clinical findings included suture material, surgery, and initial TNM stage. The US findings included shape, size, margin, echogenicity, heterogeneity, vascularity, and internal echogenic foci. The distribution, paired appearance, and "knot-and-ear" appearance of internal echogenic foci were assessed. An experiment using pork meat investigated the US configuration of suture knots.
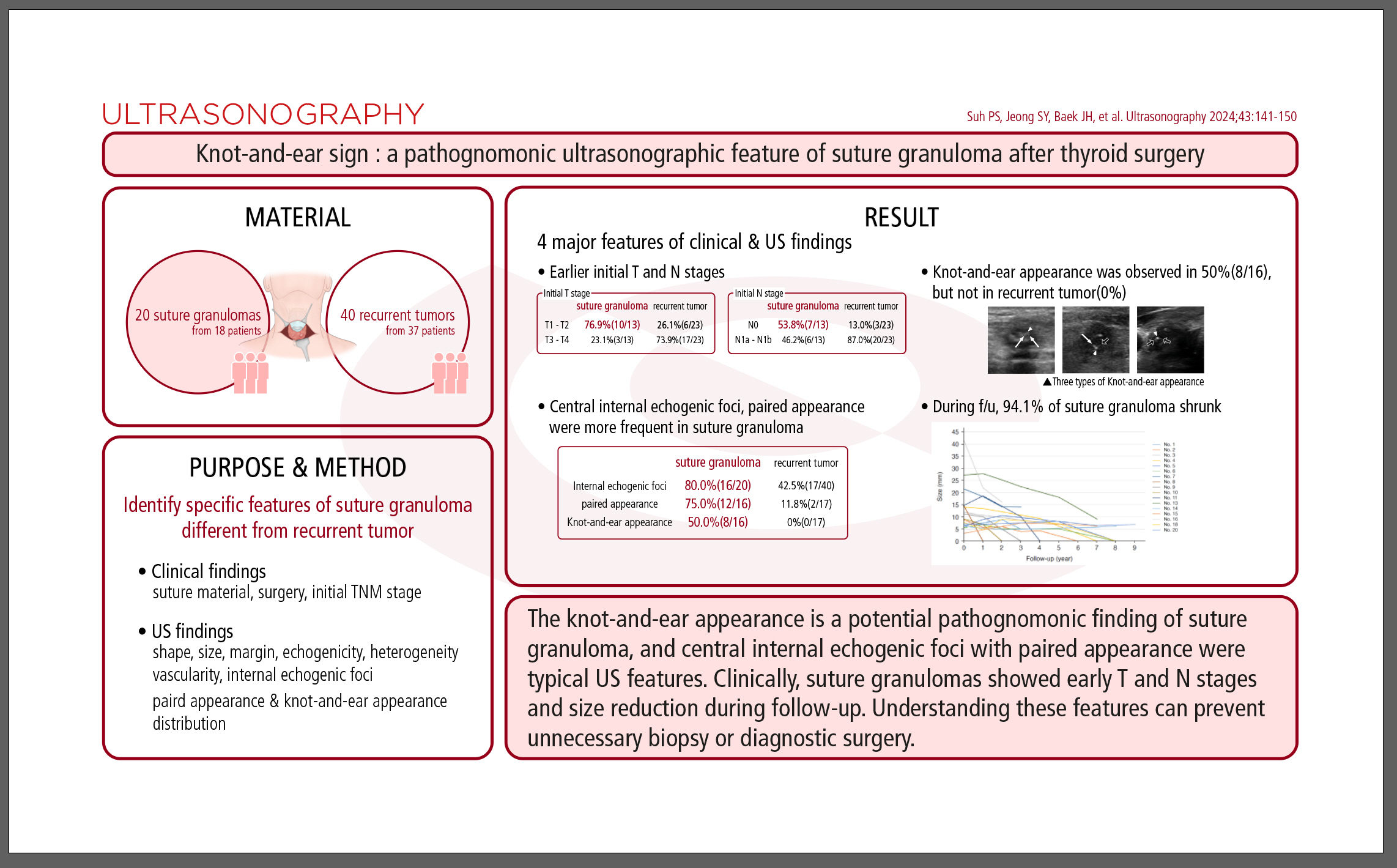
ResultsEighteen patients with 20 suture granulomas (15 women; mean age, 52±13 years) and 37 patients with 40 recurrent tumors (24 women; 54±18 years) were included. Patients with suture granulomas exhibited earlier initial T and N stages than those with recurrent tumors. The knot-and-ear appearance, defined as an echogenic dot accompanied by two adjacent echogenic dots or lines based on experimental findings, was observed in 50% of suture granulomas, but not in recurrent tumors (P<0.001). Central internal echogenic foci (68.8%, P=0.023) and paired appearance (75.0%, P<0.001) were more frequent in suture granulomas. During follow-up, 94.1% of suture granulomas shrunk.
ConclusionThe knot-and-ear appearance is a potential pathognomonic finding of suture granuloma, and central internal echogenic foci with paired appearance were typical US features. Clinically, suture granulomas showed early T and N stages and size reduction during follow-up. Understanding these features can prevent unnecessary biopsy or diagnostic surgery.
The incidence of thyroid cancer has increased worldwide [1]. After thyroidectomy, ultrasonography (US) is widely used for detecting local recurrence or cervical lymph node metastasis in the thyroidectomy bed and lateral neck, where it demonstrates high sensitivity [2,3]. In the thyroidectomy bed, both recurrent tumors and benign focal lesions, such as suture granuloma, remnant thyroid tissue, reactive lymph nodes, fibrosis, and fat necrosis, may be present [4]. Suture granuloma is a benign granulomatous inflammatory lesion that often resembles a recurrent tumor. US-guided fine-needle aspiration and core-needle biopsy (CNB) are safe and accurate methods for diagnosing lesions in the thyroidectomy bed [5,6]. However, if these procedures yield inconclusive results, diagnostic surgery may be considered. To avoid unnecessary invasive diagnostic procedures, researchers have investigated the US characteristics of suture granulomas [7-9].
Suture granulomas and recurrent tumors can present with a variety of morphologies, making differentiation between them difficult using imaging techniques. Some studies have indicated that features such as an irregular shape, ill-defined margins, hypoechoic echogenicity, and heterogeneous echotexture are more likely to be associated with suture granulomas [7,10,11]. In contrast, recurrent tumors have been linked to irregular or spiculated margins in other research [8,9,12]. Shin et al. [4], however, found no significant differences in sonographic findings between recurrent and nonrecurrent lesions. Additionally, previous research has shown that suture materials may present as hyperechoic double or single lines, suggesting that linear internal echoes or double hyperechoic dots could be specific indicators of suture granuloma [13]. Nevertheless, these signs can also be present in recurrent tumors, making it impossible to definitively diagnose suture granulomas based on these features alone. As a result, most patients require a biopsy or even diagnostic surgery to exclude the possibility of tumor recurrence. It was hypothesized that representative US features of suture granulomas might relate to the surgical knot itself, rather than the granuloma; therefore, direct identification of a surgical knot within the lesion could lead to an accurate diagnosis of suture granulomas and might be a pathognomonic feature to distinguish them from recurrent tumors. To our knowledge, no published studies have investigated and evaluated the US findings of surgical knots in patients with suture granulomas. Therefore, an experimental study was performed to evaluate the sonographic characteristics of surgical knots, specifically focusing on the scan direction.
This study aimed to evaluate the clinical and US findings of suture granulomas and recurrent tumors at the thyroidectomy bed, and to define specific US characteristics of suture granulomas through an experimental study.
This retrospective study (Asan Medical Center IRB No. 2021-1769) was approved by the institutional review board of the authors’ affiliated institution, and the requirement for informed consent was waived.
The records of 194 patients who underwent CNB for thyroidectomy bed lesions between January 2010 and December 2020 were reviewed. The pathologies identified as suture granulomas included: suture granuloma (n=4) and foreign body granuloma or foreign body reaction with chronic inflammation and stromal fibrosis, which clinically suggested suture granuloma (n=14). Benign lesions other than suture granuloma (n=54), indeterminate lesions (n=2), and malignant lesions with a non-thyroid origin (n=2) were excluded. The details of the inclusion and exclusion criteria are listed in the Supplementary Method 1. A total of 18 patients with 20 suture granulomas were included. Among the patients who were confirmed to have recurrent thyroid tumors (n=118), 37 consecutive patients with a total of 40 recurrent tumors were included, which was twice the number of suture granulomas. A flow diagram of patient selection is shown in Fig. 1.
To evaluate the sonographic findings of suture materials and suture knots, an experiment was performed using pork meat. Both non-absorbable (3-0 black silk, AILEE, Busan, Korea) and absorbable (3-0 Polysorb, Covidien, Mansfield, MA, USA) suture materials were used. First, each suture material was placed linearly in a water tank and precisely scanned using US. After tying surgical knots in the pork meat, the knot ears were cut to a length of 5 mm. The pork meat with surgical knots was placed in a water tank, and US was then performed in three different planes (axial, coronal, and sagittal). A total of 120 images—comprising 20 images for each of the two suture materials with three different planes—were obtained, and the US configuration of the suture materials and suture knot were evaluated. US was performed using an RS 85 (Samsung Medison Co., Ltd., Seoul, Korea) ultrasound system.
Medical records were reviewed, including the type of thyroidectomy, histopathologic result, initial TNM stage at the time of diagnosis, and history of radioiodine treatment. Laboratory findings at the time of initial detection on US were also reviewed, including serum thyroglobulin (Tg), thyroid-stimulating hormone, and anti-Tg antibody.
The US findings were reviewed by a radiologist with 8 years of clinical experience in performing and evaluating thyroid US images (P.S.S.) and established a consensus with an experienced radiologist with 25 years of experience in thyroid imaging (J.H.B.). The images were analyzed in a blinded manner, without access to patient information. The US findings of the lesions included the maximum diameter, shape (ovoid/round, irregular, and taller-than-wide), heterogeneity (homogeneous and heterogeneous), margin (smooth, ill-defined, and speculated), echogenicity (hyperechoic, isoechoic, hypoechoic, and markedly hypoechoic), presence of vascularity, and internal echogenic foci. The expected usual echogenicity of normal thyroid tissue was taken as the reference echogenicity for the lesion. Changes in the size of lesions (including initial detection and disappearance) during follow-up were also evaluated. The US examinations were performed using RS 85 (Samsung Medison Co. Ltd.), EPIQ7 (Philips Healthcare, Bothell, WA, USA), and Acuson S3000 (Siemens, Erlangen, Germany) systems using a linear, high-frequency probe (3-12, 5-12, and 6-18 MHz, respectively).
When there were internal echogenic foci, the number (1 or ≥2), size (≤1 mm or >1 mm), shape (round, linear, or both), distribution (central, peripheral, or diffuse), and presence of a paired appearance were evaluated, according to the reported sonographic findings of suture granuloma [7,12]. The presence of a "knot-and-ear" appearance, defined as a round internal echogenic focus accompanied by two adjacent smaller echogenic dots or lines based on the experimental findings, was also assessed.
The statistical analysis was performed using SPSS (version 21.0 for Windows, IBM Corp., Armonk, NY, USA). The Pearson chi-square test and Fisher exact test were used to compare clinical and sonographic findings between suture granulomas and recurrent tumors. The Mann-Whitney U test was used to compare patient age and the size of lesions. A P-value less than 0.05 was considered indicative of a statistically significant difference.
The demographic and clinical characteristics of the study patients are summarized in Table 1. The study included a total of 18 patients with 20 suture granulomas (83.3% women; mean age, 52.4±12.8 years) and 37 patients with 40 recurrent tumors (64.9% women; mean age, 53.7±18.3 years). All patients with recurrent tumors (100%) underwent total thyroidectomy, while only seven (38.9%) of the patients with suture granulomas underwent thyroid lobectomy (P<0.001). Initial staging was not available for five patients because they had undergone surgery at other hospitals more than 10 years prior. Of the 13 patients with suture granulomas who had available initial staging, 10 (76.9%) had initial lesions confined to the thyroid parenchyma (T1 or T2 stage), and seven (53.8%) were N0. Among the 23 patients with recurrent tumors who had available initial staging, 17 (73.9%) exhibited extrathyroidal extension (T3 or T4), and 20 (87.0%) had lymph node metastasis (N1a or N1b). The initial T and N stages were significantly different between the two groups (P=0.006 for T stage; P=0.004 for N stage).
Information on the suture materials used in the thyroidectomy bed was available for 10 patients (Table 2). Non-absorbable braided multifilament suture material (black silk) was used in seven patients, whereas absorbable braided multifilament suture material (Vicryl) was used in three patients. Information on suture materials was not available for eight patients, seven of whom underwent surgery at an outside hospital or abroad, and one who underwent surgery at the authors’ affiliated institution 17 years previously.
Both absorbable (Polysorb) and non-absorbable (black silk) suture materials appeared as double echogenic lines in the water tank, making it impossible to distinguish between the two types on US. Surgical knots tied in pork meat presented as a round echogenic dot (representing the knot) accompanied by two linear echogenic lines (representing the "ears"). Additionally, surgical knots could also be visualized as an echogenic dot with a single linear echogenic line or as echogenic dots alone, depending on the angle of the ultrasound scan. Based on these findings, a "knot-and-ear" appearance as an echogenic dot (knot) accompanied by two adjacent echogenic dots or lines (ears). The US appearance of suture materials and a surgical knot in the experimental study is illustrated in Fig. 2.
The US findings of suture granulomas and recurrent tumors are shown in Table 3. On average, suture granulomas (14.5±9.3 mm; range, 5.4 to 23.6 mm) were larger than recurrent tumors (9.7±4.6 mm; range, 3.1 to 14.3 mm; P=0.047). On US, suture granulomas more frequently showed an irregular shape (n=17, 85.0%), an ill-defined (n=11, 55.0%) or spiculated margin (n=8, 40.0%), markedly hypoechoic echogenicity (n=13, 65.0%), heterogeneous echotexture (n=19, 95.0%), no vascularity (n=16, 80.0%), and internal echogenic foci (n=16, 80.0%).
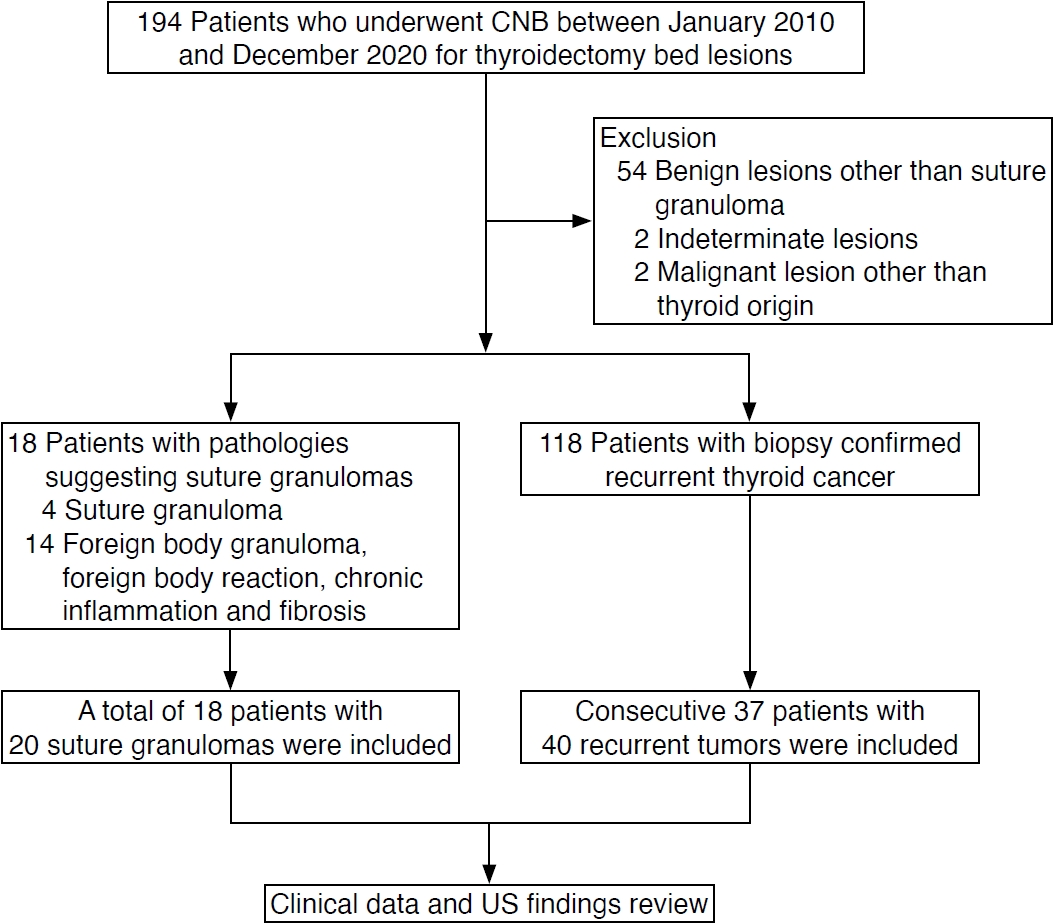
The characteristics of internal echogenic foci were also evaluated. Internal echogenic foci were more frequently observed in suture granulomas (n=16, 80.0%) than in recurrent tumors (n=17, 42.5%; P=0.007). The knot-and-ear appearance was observed in 50.0% (8/16) of suture granulomas, whereas it was not exhibited in recurrent tumors (0%, P<0.001). Cases of suture granuloma that demonstrated the three types of knot-and-ear appearance are shown in Fig. 3. The paired appearance more frequently appeared in suture granulomas (75.0%, 12/16) than in recurrent tumors (11.8%, 2/17; P<0.001); however, aggregated microcalcifications were misinterpreted as the paired appearance in two recurrent tumors (Fig. 4). Internal echogenic foci were more centrally distributed in suture granulomas (68.8%, 11/16) than in recurrent tumors (29.4%, 5/17). Peripherally distributed internal echogenic foci were not seen in suture granulomas, but they were observed in five recurrent tumors (29.4%, 5/17).
Among the 20 suture granulomas, three lesions were surgically resected, and one of these underwent diagnostic surgery despite the biopsy result. The remaining 17 lesions underwent sonographic follow-up after CNB. The mean follow-up period was 67 months. During follow-up, eight lesions (47.1%) increased in size. However, the size had decreased in 16 lesions (94.1%) by the last follow-up, and nine lesions (52.9%) had disappeared. As the suture granulomas resolved, the echogenic suture materials within the granulomas also disappeared. Four suture granulomas (23.5%) persisted for more than 7 years (Supplementary Fig. 1). In one case, a recurrent tumor developed in the suture granuloma. The maximal diameter of the suture granuloma gradually decreased during follow-up, but a round configuration with internal vascularity was suspected at the periphery of the lesion. CNB was performed, and the suspected lesion was confirmed as a recurrent tumor (Supplementary Fig. 2).
This study demonstrated that 50% of suture granulomas showed a distinctive knot-and-ear appearance, which was not observed in any recurrent tumors (P<0.001). This characteristic appearance directly indicated the presence of a surgical knot within the granuloma, which was reproduced in the experimental study and may be a pathognomonic finding of suture granuloma. Additionally, centrally distributed internal echogenic foci with a paired appearance were typical US features of suture granuloma. Other ancillary clinical characteristics, such as initial early T and N stages and a gradual size reduction during follow-up, may also be helpful for differentiating suture granulomas from recurrent tumors. Understanding these US and clinical features of suture granuloma can prevent unnecessary biopsy or even diagnostic surgery.
A suture granuloma is composed of suture material within a surrounding granuloma, and distinguishing its US features from those of recurrent tumors can be challenging [4]. In the experimental component of this study, it was observed that the ears of the suture knot appeared as either linear echogenic lines or dots, depending on the scanning plane. In accord with these findings, it was observed that surgical knots within suture granulomas frequently demonstrated this characteristic knot-and-ear appearance, typically appearing as an echogenic dot accompanied by two adjacent echogenic dots or lines. Therefore, the identification of a knot-and-ear appearance, which directly indicates suture materials within suture granulomas, can prevent unnecessary biopsy or diagnostic surgery. In this study, CNB was performed in all patients to exclude recurrence, and additional diagnostic surgery was performed in one patient. For lesions highly suggestive of suture granuloma with a knot-and-ear appearance, serial follow-up US and observation of size changes are recommended.
Another finding of internal echogenic foci suggesting suture granuloma was the paired appearance. The experimental study showed that the suture material itself appeared as echogenic double lines on the longitudinal direction scan, irrespective of the type of suture material (either absorbable or non-absorbable). Similarly, Thomas et al. reported that both braided and monofilament suture materials appeared as rail-like hyperechoic lines on longitudinal scans and showed a paired appearance on transverse scans [13]. Kim et al. [7] reported that the paired appearance was found in 92% of suture granulomas, suggesting that this is an important diagnostic factor for suture granuloma. A central distribution of internal echogenic foci was also a significant US finding. Suture granulomas can develop around both absorbable and non-absorbable suture materials, most commonly around silk, as shown in our study [13-16]. They develop through chronic granulomatous foreign body reactions around retained suture materials [7,13,17-19], and as a result, the internal echogenic foci in suture granulomas show a central distribution [7,11]. However, aggregated microcalcifications within recurrent tumors may lead to a false-positive paired appearance and can also be centrally distributed. Therefore, diagnosing suture granuloma based solely on paired appearance or central internal echogenic foci, without the knot-and-ear appearance, needs cautious consideration and close follow-up.
Clinically, eight (47.1%) suture granulomas increased in size during follow-up, which may have been due to the progression of inflammatory changes. The size ultimately decreased in all but one patient, and 52.9% of lesions disappeared. Interestingly, the echogenic suture materials also disappeared during follow-up in all cases. Although silk is considered a non-absorbable suture material, it does not permanently remain in body tissue and is usually nearly absorbed within 2 years [20]. Aga et al. [8] reported that 91% of suture granulomas decreased in size, but they could remain present for 5 years at maximum. As 23.5% of the suture granulomas remained present for more than 7 years in this study, it is suggested that follow-up should be performed for several years. Additionally, tumor recurrence can develop within a suture granuloma, and in the case presented herein, this was demonstrated by a change in the US configuration of the lesion during follow-up. Furthermore, a typical US feature of suture granuloma observed in this study was the central distribution of internal echogenic foci, with none demonstrating a peripheral distribution. As a result, a change in the location of the echogenic foci to the periphery during follow-up should raise suspicion of tumor recurrence adjacent to the suture granuloma. Thus, monitoring should be continued even after a lesion is pathologically confirmed as suture granuloma. If the sonographic configuration changes during follow-up, US-guided biopsy should be performed, targeting specifically the altered area.
With respect to cancer staging, a large proportion of patients with suture granuloma were classified as low risk according to the risk stratification system of the 2015 ATA (American Thyroid Association) guidelines [21], and 38.9% underwent thyroid lobectomy. Furthermore, among those patients with suture granulomas who underwent total thyroidectomy, 81.8% showed postoperative serum Tg levels lower than 1 ng/mL, suggesting an excellent response. Clinical information including the initial stage and serum Tg level seems informative for differentiating suture granuloma from recurrent tumor.
The present study has several limitations. This is a retrospective study with a small number of cases. The number of suture granulomas confirmed pathologically was small, even with a long period of enrollment, limiting the statistical power of the study. In addition, the sonographic findings were retrospectively reviewed using previously captured images. In this study, 50% of suture granuloma showed a knot-and-ear appearance. Good depiction of the knot-and-ear appearance depends on the specific direction of the scan, as mentioned above, and the previously determined scan direction therefore presented a limitation for evaluating the knot-and-ear appearance in this retrospective study. Recently, the authors have tried to conduct scans in various planes to identify the knot-and-ear appearance of thyroid operative bed lesions in daily practice. Further prospective studies with larger numbers of cases are required to validate these results.
In conclusion, a knot-and-ear appearance may serve as a pathognomonic finding, and centrally distributed internal echogenic foci with a paired appearance are typical US features of suture granuloma. Clinically, suture granulomas showed initial early T and N stages and a gradual size reduction during follow-up. Understanding these US and clinical features of suture granuloma can prevent unnecessary biopsy or even diagnostic surgery.
NotesAuthor Contributions Conceptualization: Baek JH. Data acquisition: Suh PS, Jeong SY, Lee YM, Park YS, Ahn JY. Data analysis or interpretation: Suh PS, Baek JH. Drafting of the manuscript: Suh PS. Critical revision of the manuscript: Baek JH, Kim TY, Lee YM, Song DE, Chung SR, Choi YJ, Lee JH. Approval of the final version of the manuscript: all authors. Supplementary MaterialSupplementary Method 1.Patient selection (https://doi.org/10.14366/usg.23210).
Supplementary Fig. 1.Recurrent tumor misdiagnosed as suture granuloma on ultrasonography (https://doi.org/10.14366/usg.23210).
Supplementary Fig. 2.A 70-year-old woman with a history of left thyroid lobectomy because of papillary thyroid cancer 6 years previous, and completion thyroidectomy because of recurrence 4 years previous (https://doi.org/10.14366/usg.23210).
References1. Roman BR, Morris LG, Davies L. The thyroid cancer epidemic, 2017 perspective. Curr Opin Endocrinol Diabetes Obes 2017;24:332–336.
2. do Rosario PW, Fagundes TA, Maia FF, Franco AC, Figueiredo MB, Purisch S. Sonography in the diagnosis of cervical recurrence in patients with differentiated thyroid carcinoma. J Ultrasound Med 2004;23:915–920.
3. Lee YH, Lee NJ, Kim JH, Song JJ. US diagnosis of cervical recurrence in patients operated on thyroid cancer: sonographic features and clinical significance. Auris Nasus Larynx 2007;34:213–219.
4. Shin JH, Han BK, Ko EY, Kang SS. Sonographic findings in the surgical bed after thyroidectomy: comparison of recurrent tumors and nonrecurrent lesions. J Ultrasound Med 2007;26:1359–1366.
5. Bishop JA, Owens CL, Shum CH, Ali SZ. Thyroid bed fine-needle aspiration: experience at a large tertiary care center. Am J Clin Pathol 2010;134:335–339.
6. Jeong SY, Baek JH, Chung SR, Choi YJ, Song DE, Chung KW, et al. Diagnostic performance of core needle biopsy for characterizing thyroidectomy bed lesions. Korean J Radiol 2022;23:1019–1027.
7. Kim JH, Lee JH, Shong YK, Hong SJ, Ko MS, Lee DH, et al. Ultrasound features of suture granulomas in the thyroid bed after thyroidectomy for papillary thyroid carcinoma with an emphasis on their differentiation from locally recurrent thyroid carcinomas. Ultrasound Med Biol 2009;35:1452–1457.
8. Aga H, Hirokawa M, Suzuki A, Ota H, Oshita M, Kudo T, et al. Sonographic evaluation of nodules newly detected in the neck after thyroidectomy: suture granuloma versus recurrent carcinoma. Ultrasound Int Open 2018;4:E124–E130.
9. Zaheer S, Tan A, Ang ES, Loke KS, Kao YH, Goh A, et al. Post-thyroidectomy neck ultrasonography in patients with thyroid cancer and a review of the literature. Singapore Med J 2014;55:177–182.
10. Kamaya A, Gross M, Akatsu H, Jeffrey RB. Recurrence in the thyroidectomy bed: sonographic findings. AJR Am J Roentgenol 2011;196:66–70.
11. Langer JE, Luster E, Horii SC, Mandel SJ, Baloch ZW, Coleman BG. Chronic granulomatous lesions after thyroidectomy: imaging findings. AJR Am J Roentgenol 2005;185:1350–1354.
12. Ko MS, Lee JH, Shong YK, Gong GY, Baek JH. Normal and abnormal sonographic findings at the thyroidectomy sites in postoperative patients with thyroid malignancy. AJR Am J Roentgenol 2010;194:1596–1609.
13. Rettenbacher T, Macheiner P, Hollerweger A, Gritzmann N, Weismann C, Todoroff B. Suture granulomas: sonography enables a correct preoperative diagnosis. Ultrasound Med Biol 2001;27:343–350.
14. Javalgi AP, Arakeri SU. Post thyroidectomy suture granuloma: a cytological diagnosis. J Clin Diagn Res 2013;7:715–717.
15. Matsuura S, Sasaki K, Kawasaki H, Abe H, Nagai H, Yoshimi F. Silk suture granuloma with false-positive findings on PET/CT accompanied by peritoneal metastasis after colon cancer surgery. Int J Surg Case Rep 2016;28:22–25.
16. Imperiale L, Marchetti C, Salerno L, Iadarola R, Bracchi C, Vertechy L, et al. Nonabsorbable suture granuloma mimicking ovarian cancer recurrence at combined positron emission tomography/computed tomography evaluation: a case report. J Med Case Rep 2014;8:202.
17. Chung YE, Kim EK, Kim MJ, Yun M, Hong SW. Suture granuloma mimicking recurrent thyroid carcinoma on ultrasonography. Yonsei Med J 2006;47:748–751.
18. Rosenberg N, Moolten SE, Vroman L. Tissue reactions to waxes derived from spool cotton; possible etiologic relation to suture granulomas and suture extrusion. Arch Surg (1920) 1950;60:363–371.
19. Rosenberg D, Schechtmann M. Granuloma of the stomach caused by a foreign body (cotton thread suture). Rev Paul Med 1963;62:325–332.
20. Chu CC, von Fraunhofer JA, Greisler HP. Wound closure biomaterials and devices. Boca Raton, FL: CRC Press, 2018.
21. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1–133.
Experimental evaluation of the ultrasonographic (US) findings of surgical knots using pork meat imaged in three different planes, showing the US examinations of (A, B) absorbable (Polysorb) and (C, D) non-absorbable (black silk) suture materials.A, C. The suture materials show linear double echogenic lines on longitudinal scans, which are associated with a paired appearance in suture granuloma. B, D. The suture knots show a different configuration according to the scanning plane, presenting a knot-and-ear appearance (left), an echogenic dot with a single linear echogenic line (middle), or only echogenic dots (right).
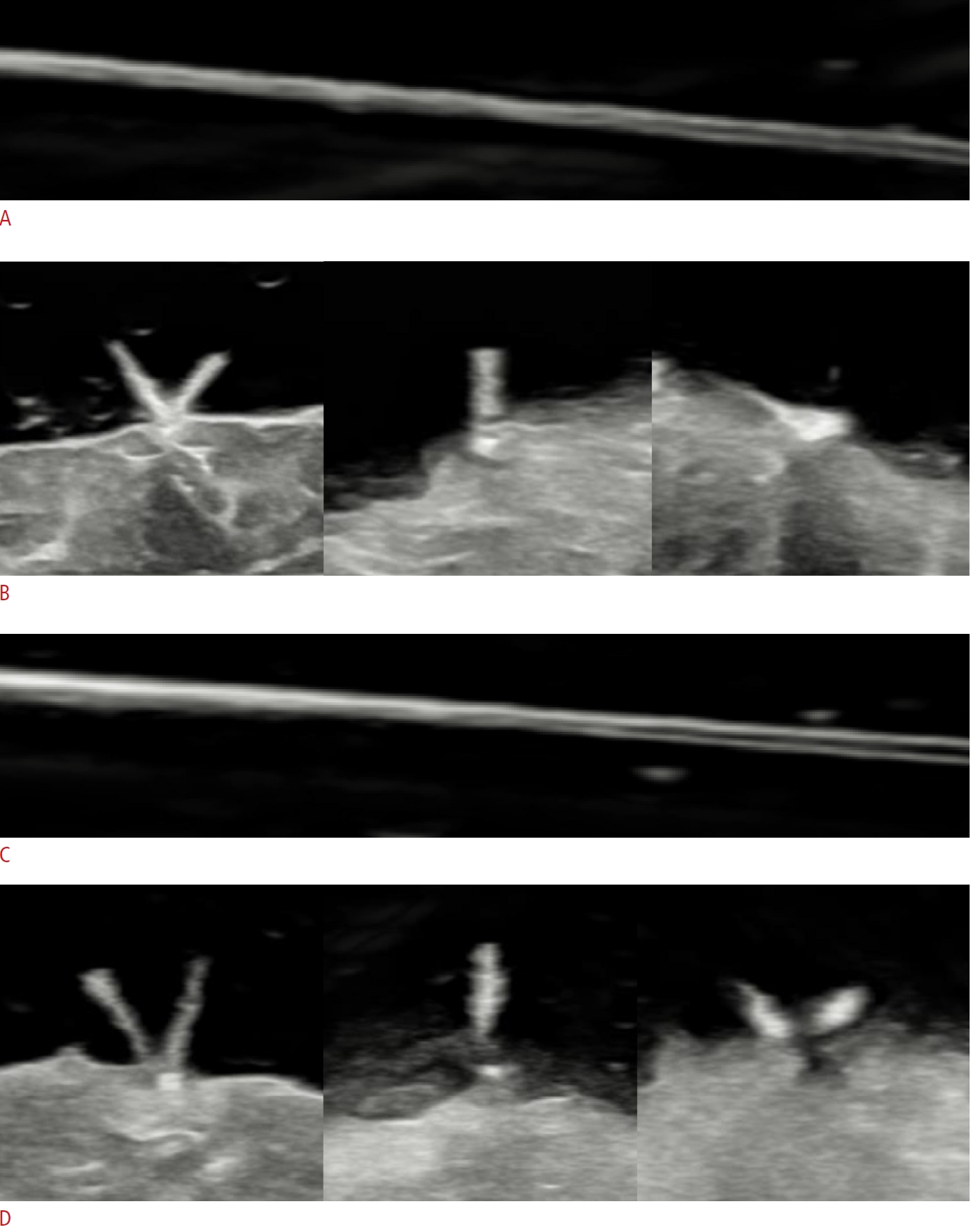 Fig. 2.Three types of knot-and-ear appearance according to the length of the ear in eight patients with suture granulomas.A-F. The first type of the knot-and-ear appearance shows an echogenic dot (knot, arrowheads) accompanied by two adjacent smaller echogenic dots (ears, arrows). G-I. The second type presents as an echogenic dot (arrowheads) accompanied by an adjacent echogenic line (open arrows) and one echogenic dot (arrows). J, K. The third type shows an echogenic dot (arrowhead) accompanied by two adjacent echogenic lines (open arrows).
 Fig. 3.Recurrent tumor misdiagnosed as a suture granuloma on ultrasonography.A, B. Recurrent tumors in the thyroid bed after thyroidectomy show internal echogenic foci with a paired appearance (arrows).
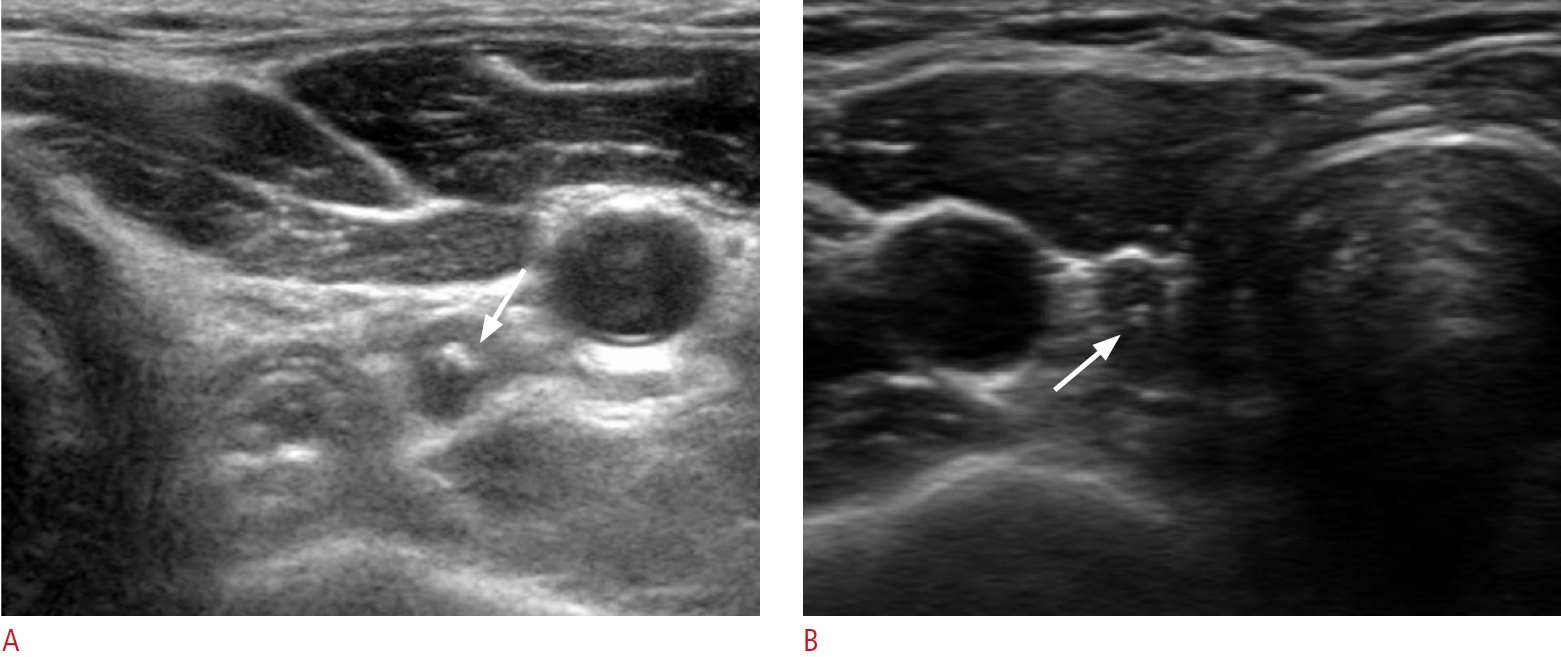 Fig. 4.Table 1.Demographic and clinical characteristics of the study patients
Table 2.Demographic and clinical findings of the patients with suture granulomas Table 3.Characteristics and sonographic findings of the lesions
|



 Print
Print facebook
facebook twitter
twitter Linkedin
Linkedin google+
google+
 Download Citation
Download Citation PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI




